Session Information
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Often not evaluated in clinical visits, financial distress associated with medical costs, also known as financial toxicity, has emerged as an important factor affecting health due to reduced adherence, stress, and other negative impacts. The Functional Assessment of Chronic Illness Therapy – Comprehensive Score for Financial Toxicity (FACIT-COST) patient-reported outcome measure provides a quantitative measure of financial distress validated in chronic diseases such as cancer, diabetes and cardiovascular disease. To our knowledge, financial distress has never been described in rheumatoid arthritis (RA). We aimed to quantify financial distress and identify its determinants in participants with rheumatoid arthritis (RA) in comparison to non-inflammatory musculoskeletal disease (NIMSKD).
Methods: We identified adult respondents enrolled in the FORWARD registry who had RA or NIMSKD and completed the FACIT-COST questionnaire. In this cross-sectional study, the FACIT-COST score was analyzed as a continuous variable (higher score indicates less financial distress) and as a binary variable (presence of financial distress with threshold < 26). Double LASSO was applied to linear and logistic regression to select best multivariable models evaluating associations between financial distress and predictors.
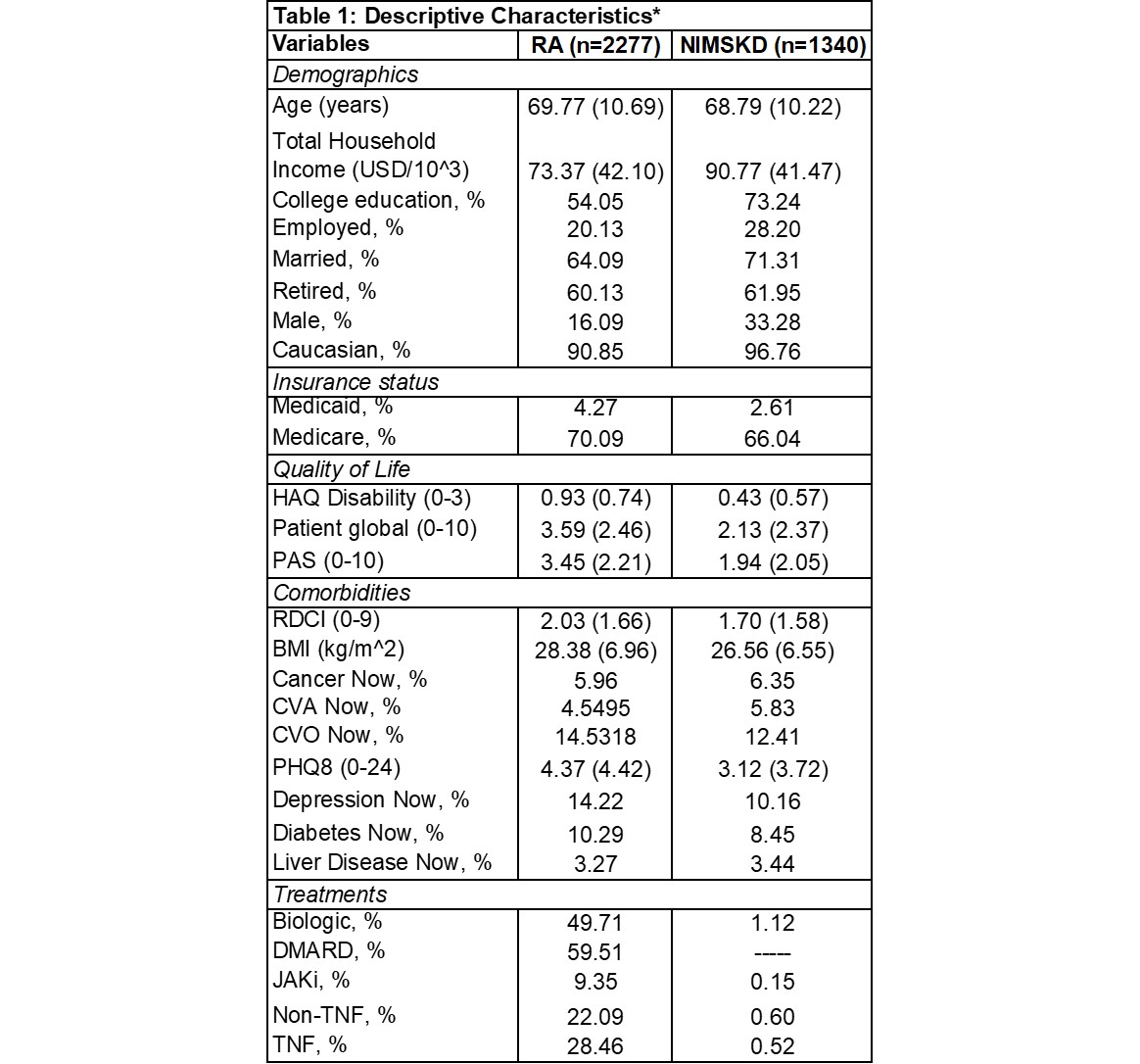
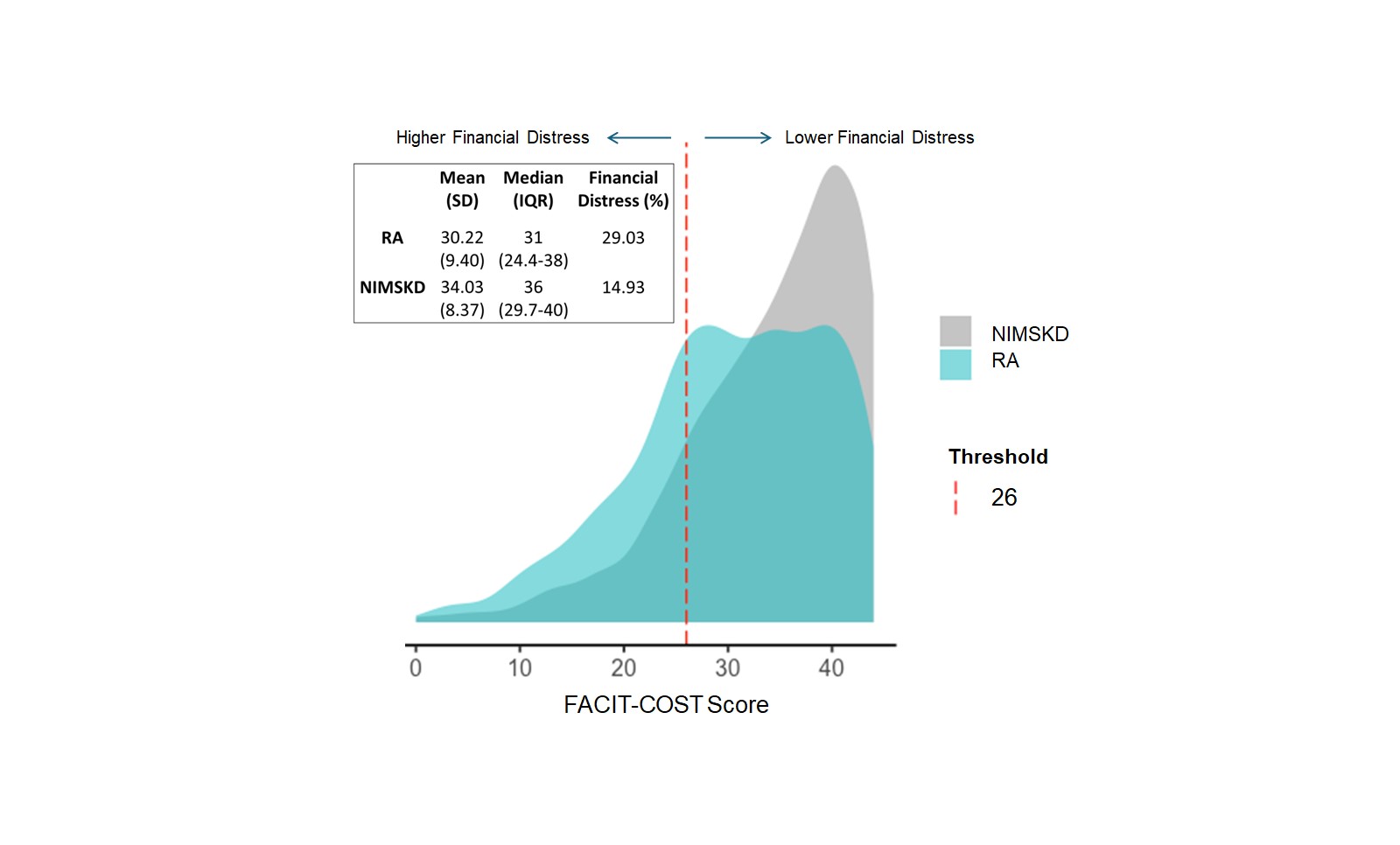
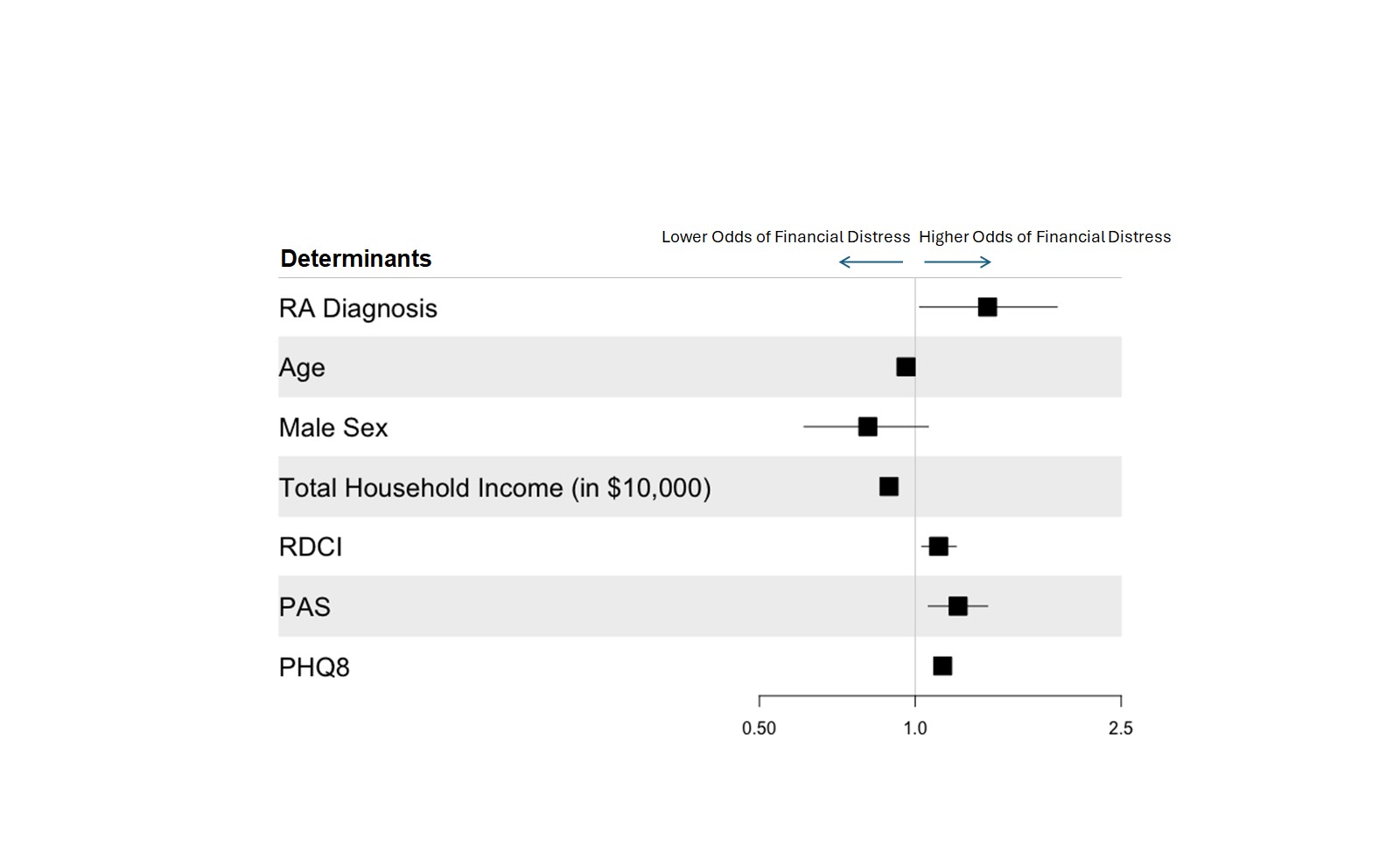
Results: A total of 3617 patients were included in the sample and analyzed in two diagnosis groups, RA (n=2277) and NIMSKD (n=1340) (Table 1). RA patients (n=2277) had lower FACIT-COST scores indicative of more financial distress than patients with NIMSKD (n=1340) with mean (SD) scores of 30.2 (9.4) and 34.0 (8.4), respectively (unadjusted-p< 0.001) (Figure 1). Financial distress was also more frequent in RA than NIMSKD (29% vs. 15%; unadjusted-p< 0.001). Differences in financial distress by diagnosis persisted following multivariable adjustment. In univariate analyses, younger age, lower household income, less frequent college education, being married, being retired, male sex, and Caucasian race were associated with presence of financial distress in patients with RA. In multivariable logistic regression models, determinants of financial distress in patients with RA included depression (aOR 1.13; 95% CI 1.09-1.16) and disease severity (aOR 1.21; 95% CI 1.13-1.28)) (Figure 2). Notably, use of biologic or targeted synthetic disease-modifying anti-rheumatic drugs were not associated with financial distress in adjusted models. Among those with RA, determinants identified in multivariable models were similar whether financial distress was examined as a binary or continuous outcome.
Conclusion: Financial distress is prevalent in patients with RA and appears to be greatest in those with comorbidities, specifically depression. Future prospective studies are needed to examine causal directionality to elucidate whether future interventions aimed at comorbid conditions might result in clinical benefit through reductions in financial distress.
Values are odds ratios with 95% Confidence Intervals. Similar predictors selected in disease specific multivariable models. Expensive therapies utilized in RA treatment do not significantly increase odds for financial distress.
To cite this abstract in AMA style:
Brown Keebler A, Im Y, Pedro S, Mikuls T, Peters E, Michaud K. Financial Distress and Its Determinants in Adults with Rheumatoid Arthritis [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/financial-distress-and-its-determinants-in-adults-with-rheumatoid-arthritis/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/financial-distress-and-its-determinants-in-adults-with-rheumatoid-arthritis/