Session Information
Date: Sunday, November 5, 2017
Title: Rheumatoid Arthritis – Clinical Aspects Poster I: Treatment Patterns and Response
Session Type: ACR Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose:
The management plan for rheumatoid arthritis (RA) might be a relatively simple task if only disease activity is considered but might become more complex when additional factors are considered.
Previously, in a real clinical setting of RA outpatients, we explored the impact of musculoskeletal ultrasound, added to clinical evaluations in the treatment decision; we found that ultrasound had a greater impact in the trainee (TR) than in the senior rheumatologist (SR).
The aim of the present study was to investigate which factors impact the treatment recommendation in RA outpatients and to detect potential differences among 2 rheumatologists categorized by their experience, TR vs. SR.
Methods:
Eighty-five consecutive and randomly selected RA outpatients underwent 170 assessments, 85 each by the SR and the TR. Initially, both physicians performed a complete rheumatic assessment which included disease activity as per DAS28 and recommended a treatment. Then, the patients underwent a musculoskeletal evaluation by an independent rheumatologist. In the final step, the TR and the SR integrated ultrasound findings with their previous evaluation and reviewed their recommendations. In addition, immediately after each patient encounter, both physicians were instructed to select and rate, which among the following factors were determinant in the final treatment proposal: clinical assessments, ultrasound findings, comorbidities, treatment related adverse events, costs/availability, patient«s preference and DMARD maximum dose. In all the instances, the SR and the TR were blinded to each other assessments. Data were obtained on standardized formats. Descriptive statistics were used. The study was approved by the local IRB and all the patients signed informed consent.
Results:
Patients were primary middle-aged (mean±SD: 45.1 ± 12.4 years) female (91.4%) and had disease duration of 7.5±3.9 years. The majority of the patients were in DAS28 remission (<2.6) and 24 (28.2%) showed some disease activity. All the patients were on DMARDs and 48% had additional low doses of oral corticosteroids.
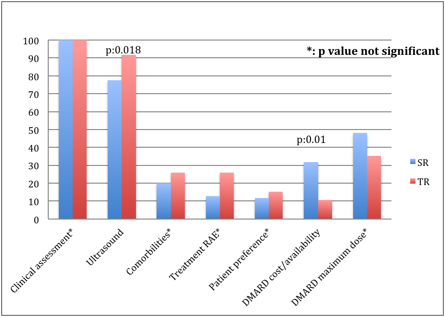
Clinical assessments were rated as determinants in the totality of the clinical scenarios, followed by ultrasound findings in 84.7%, DMARD maximum dose in 41.2%, comorbidities in 23%, DMARD cost/availability in 21.2%, DMARD-related adverse events in 20% and finally, patient preference was rated as determinant in 14.1% of the clinical scenarios. Interestingly, the SR and the TR differed in the selection of the factors they considered determinant for the treatment proposal (Figure).
Conclusion:
Disease activity drives the treatment decision during RA patients follow-up, although additional factors may be considered. Considerable variation was observed in how doctors rated those factors and these variations depended on physician«s experience.
Figure
To cite this abstract in AMA style:
Sifuentes-Cantú C, Contreras-Yañez I, Saldarriaga Rivera L, Lozada AC, Gutierrez M, Pascual-Ramos V. Factors That Drive Treatment Recommendation during Rheumatoid Arthritis Patient´s Follow-up, Differ According to Physician Experience [abstract]. Arthritis Rheumatol. 2017; 69 (suppl 10). https://acrabstracts.org/abstract/factors-that-drive-treatment-recommendation-during-rheumatoid-arthritis-patients-follow-up-differ-according-to-physician-experience/. Accessed .« Back to 2017 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/factors-that-drive-treatment-recommendation-during-rheumatoid-arthritis-patients-follow-up-differ-according-to-physician-experience/