Session Information
Date: Saturday, November 12, 2022
Title: SLE – Diagnosis, Manifestations, and Outcomes Poster I: Diagnosis
Session Type: Poster Session A
Session Time: 1:00PM-3:00PM
Background/Purpose: Lupus nephritis (LN) is one of the most severe manifestations of systemic lupus erythematosus (SLE). Approximately 10 to 30% of patients with LN progress to end-stage renal disease (ESRD) within ten years. Increasing evidence has shown that tubulointerstitial injury, especially interstitial fibrosis/tubular atrophy (IFTA), is a strong predictor of progression to ESRD. However, factors associated with worsening IFTA on repeat kidney biopsy are not well studied. The objective of this study was to evaluate the demographic, clinical, and histopathological factors associated with progression from none-mild IFTA on index kidney biopsy to moderate-severe IFTA on clinically indicated repeat kidney biopsy in LN patients.
Methods: We identified patients with SLE by the 1997 American College of Rheumatology (ACR) or the Systemic Lupus Erythematosus International Collaborating Clinics (SLICC) criteria who underwent an index kidney biopsy between 1997 and 2020. Patients with LN Class I, II, III, IV, V, and mixed LN based on the 2003 International Society of Nephrology (ISN) and the Renal Pathology Society (RPS) classification on index biopsy who underwent a clinically indicated repeat kidney biopsy were identified. Chart reviews were performed to obtain demographic, clinical and histopathological data. None-mild IFTA was defined as less than 25% acreage of the interstitium affected by fibrosis and atrophy, and moderate-severe IFTA was defined as equal to or greater than 25% of the interstitium affected. Patients who had none-mild IFTA on index biopsy and progressed to moderate-severe IFTA on repeat biopsy were defined as progressors. Patients with none-mild IFTA on both biopsies were defined as non-progressors.
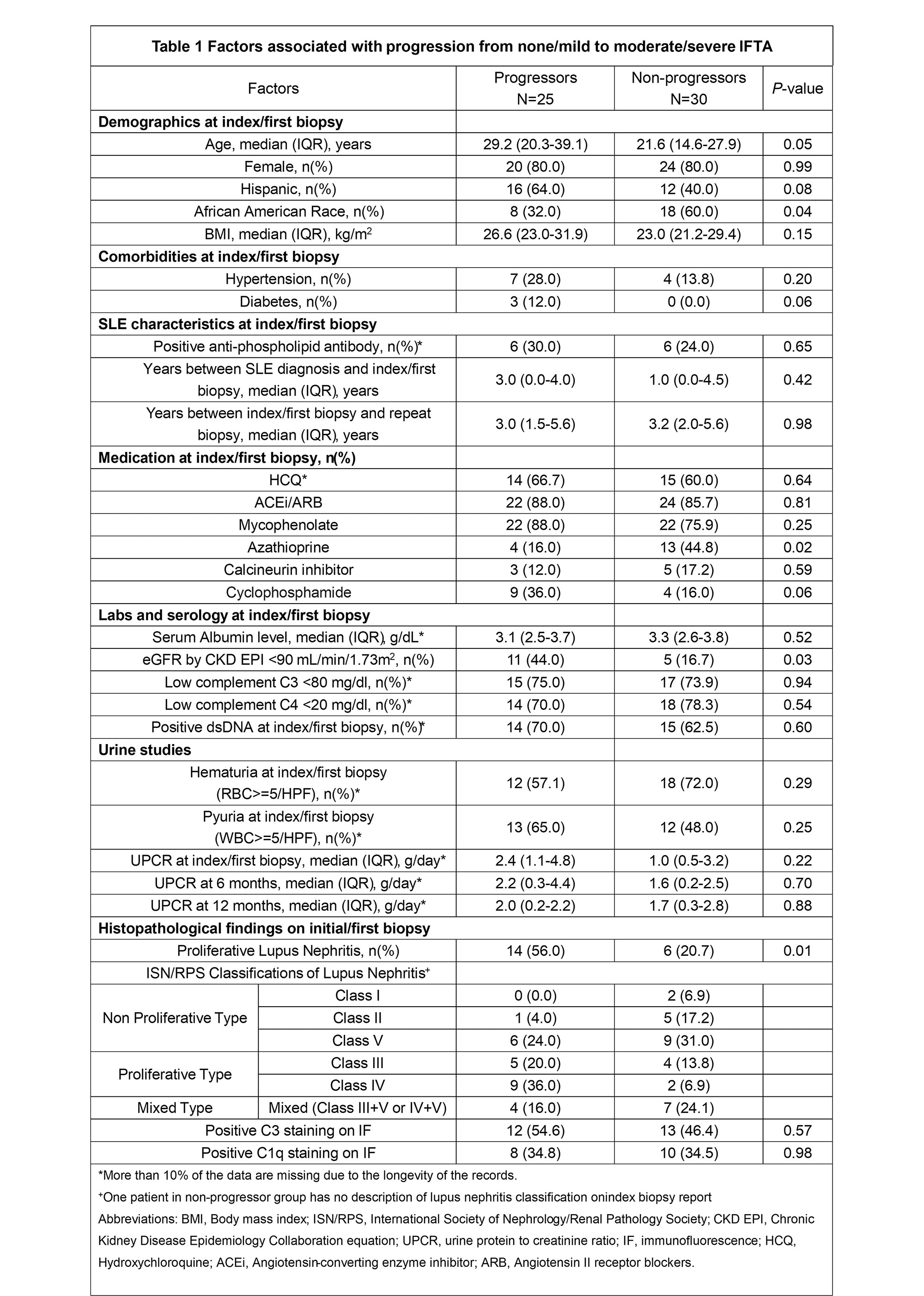
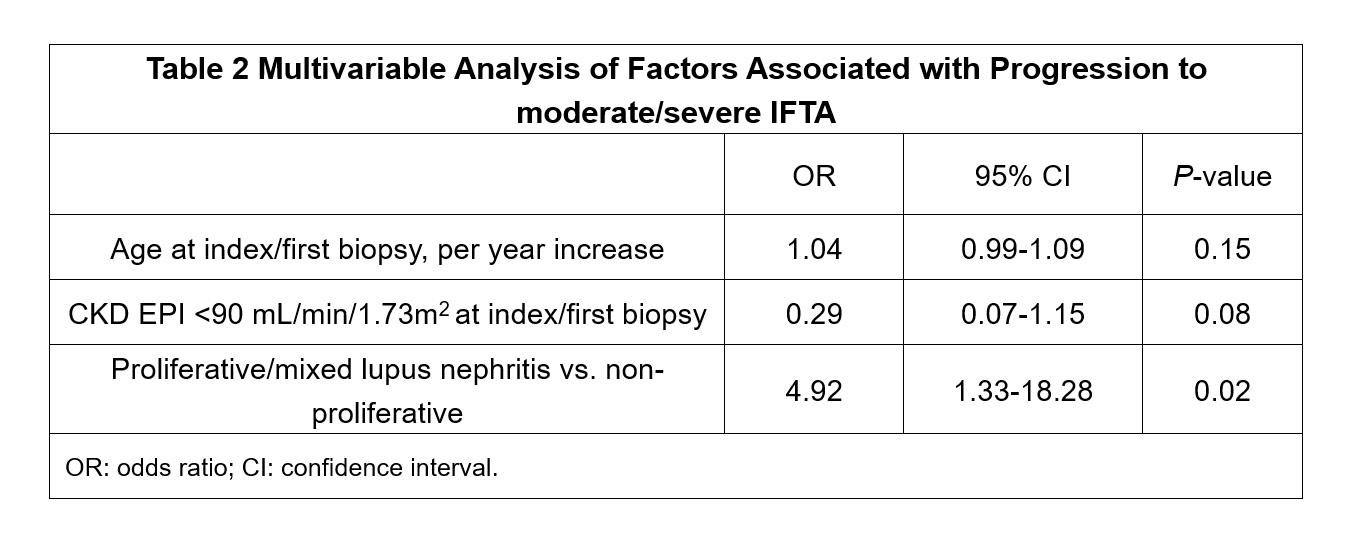
Results: Of the 150 SLE patients with biopsy-proven LN, 55 underwent a clinically indicated repeat kidney biopsy. Of these 55 patients included in this study, 44 (80%) were women, 26 (43%) self-identified as Black or African American, and 28 (51%) self-identified as Hispanic or Latino. Twenty-five (45%) progressed from none-mild to moderate-severe IFTA. Compared to non-progressors (Table 1), progressors were older (median age 29.2 [20.3-39.1] vs. 21.6 [14.6-27.9] years old, p=0.05), included a higher proportion of patients with low eGFR (CKD EPI < 90 mL/min/1.73m2) (11 [44%] vs. 5 [17%], p=0.03) and proliferative LN (14 [56%] vs. 6 [21%], p=0.01). Progressors included a lower proportion of Black or African American patients (8 [32%] vs 18 [60%], p=0.04) and a lower proportion of patients receiving Azathioprine (4 [16%] vs. 13 [45%], p=0.02). There was no difference between the two groups with regards to median years from index to repeat biopsy, hypertension, diabetes, low serum complement C3 or C4, or immunofluorescence (IF) staining of C1q or C3 on index biopsy. The multivariable logistic regression analysis (Table 2) showed that proliferative LN was associated with IFTA progression (OR 4.92, 95% CI 1.33-18.28, p=0.02).
Conclusion: Proliferative LN was associated with a higher risk of IFTA progression, suggesting that glomerular damage is one of the major drivers of IFTA progression in SLE.
1. Londoño Jimenez et al., Tubulointerstitial Damage in Lupus Nephritis: A Comparison of the Factors Associated With Tubulointerstitial Inflammation and Renal Scarring. Arthritis & Rheumatology, 70(11), 1801–1806.
2. Leatherwood, C. et al., Clinical characteristics and renal prognosis associated with interstitial fibrosis and tubular atrophy (IFTA) and vascular injury in lupus nephritis biopsies. Seminars in arthritis and rheumatism, 49(3), 396–404.
3. Kwon, O. C. et al., Factors associated with aggravation of tubulointerstitial damage on repeated biopsies in lupus nephritis patients with treatment failure. Clinical and experimental rheumatology, 38(2), 239–244.
To cite this abstract in AMA style:
Shao D, Londoño Jimenez A, Salgado Guerrero M, Broder A, Wang S. Factors Associated with Worsening Interstitial Fibrosis/Tubular Atrophy in Lupus Nephritis Patients Undergoing Repeat Kidney Biopsy [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/factors-associated-with-worsening-interstitial-fibrosis-tubular-atrophy-in-lupus-nephritis-patients-undergoing-repeat-kidney-biopsy/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/factors-associated-with-worsening-interstitial-fibrosis-tubular-atrophy-in-lupus-nephritis-patients-undergoing-repeat-kidney-biopsy/