Session Information
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Lupus lesional skin has elevated interferon expression, is highly colonized with Staphylococcus aureus (50%) and has no FDA-approved treatment options. S. aureus is known to induce proinflammatory responses such as cytokine expression and infiltration of immune cells to the affected area. Thus dysbiosis of the cutaneous microbiota could negatively affect the cutaneous immune response. Here we investigated the effect of topical antibiotic on lupus lesional skin to determine whether it affects inflammatory gene expression.
Methods: Adult Systemic Lupus Erythematosus (SLE) patients with skin inflammation (discoid or subacute cutaneous lupus erythematosus lesions) were recruited for this study from the Michigan Lupus cohort. The study was approved by the University of Michigan IRB and all patients gave informed consent. Lesions were swabbed to determine S. aureus colonization and then 4 mm skin biopsies were collected from the affected area. Patients were then randomized for either mupirocin treatment or petroleum jelly as the control (3x each). Mupirocin is a topical antibiotic that reduces bacterial load in the treated area. Product was applied to the lesion thrice daily for 7 days followed by repeat swab and biopsy. Biopsies were saved at -80 °C until use. RNA was isolated from the biopsies, checked for quality, and sequenced to determine transcriptomic changes.
Results: Mupirocin treatment results in a greater reduction of differentially-expressed genes (DEGs) (184) when compared to treatment with petroleum jelly (133). Functional enrichment analysis of the differentially regulated genes with each treatment showed that antibiotic treatment resulted in downregulation of genes that were significantly enriched in cytokine pathways including genes such as CCL19, CCL2, CXCL10, FPR1, and PTGS2 and genes such as STAT1, OAS3, SOCS3, ICAM1 and IL6 that are interferon (IFN) regulated. In contrast, downregulated genes post petroleum jelly treatment were enriched in cell communication and extracellular matrix pathways. Importantly, a scatter plot of the data to compare the effects of the two treatments showed that DEGs from the two treatments were almost completely independent with only a few that were DE in both treatments.
Conclusion: Inflammatory signaling can be reduced in lupus lesional skin by reducing Gram-positive bacterial load by topical antibiotic treatment. CCL19 is an interferon regulated gene that mediates ectopic lymphoid aggregates in non-lymphoid tissues. CCL2, a chemokine highly expressed in CLE, and CXCL10 are known to recruit monocytes, memory T cells and dendritic cells to sites of inflammation, resulting in Th1 oriented inflammation in CLE. Thus, modulation of the lesional microbiota may facilitate reduction in inflammation. This may be particularly helpful in patients who are recalcitrant to typical treatment protocols for skin inflammation. Further study of additional patients is underway to confirm this finding.
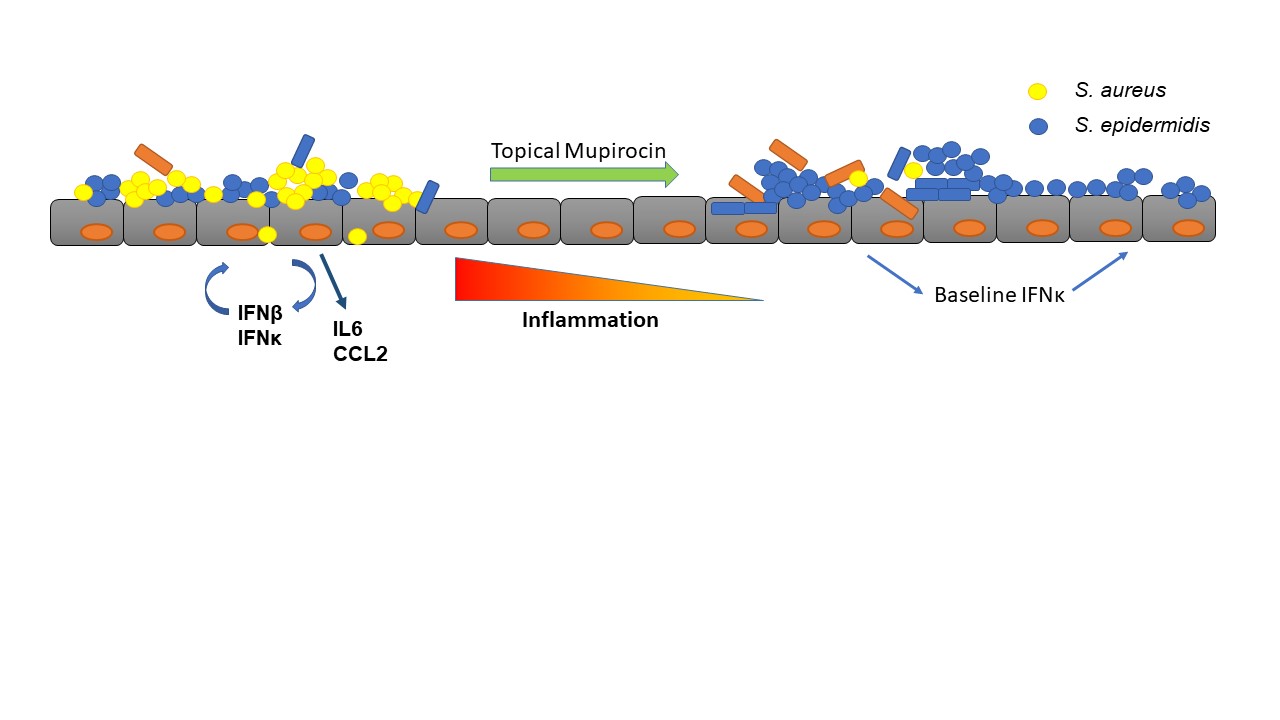 Graphical representation of lesional skin showing high IFN production that contributes to further inflammation, as well as high S. aureus colonization and low microbial diversity. Mupirocin treatment could reduce the proliferation and density of S. aureus thereby improving microbial diversity as well as reducing inflammation.
Graphical representation of lesional skin showing high IFN production that contributes to further inflammation, as well as high S. aureus colonization and low microbial diversity. Mupirocin treatment could reduce the proliferation and density of S. aureus thereby improving microbial diversity as well as reducing inflammation.
To cite this abstract in AMA style:
Sirobhushanam S, Billi A, Tsoi A, Berthier C, Gudjonsson J, Kahlenberg J. Exposure to Topical Antimicrobials Reduces Inflammatory Gene Expression in Cutaneous Lupus Lesional Skin [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/exposure-to-topical-antimicrobials-reduces-inflammatory-gene-expression-in-cutaneous-lupus-lesional-skin/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/exposure-to-topical-antimicrobials-reduces-inflammatory-gene-expression-in-cutaneous-lupus-lesional-skin/
