Session Information
Date: Tuesday, November 10, 2015
Title: Systemic Lupus Erythematosus - Clinical Aspects and Treatment V: Neuropsychiatric Lupus
Session Type: ACR Concurrent Abstract Session
Session Time: 2:30PM-4:00PM
Background/Purpose:
Neurocognitive dysfunction
is a common manifestation of childhood-onset Systemic Lupus Erythematosus
(cSLE). Murine models suggest that loss of the
blood-brain barrier (BBB) integrity allows brain-reactive proteins to enter the
CNS and contribute to SLE-associated pathology. Contrast magnetic resonance
imaging (MRI) can provide a measure of BBB integrity, but has risk associated
with gadolinium use. We have previously identified multiple areas of gray
matter (GM) loss on structural MRI in cSLE patients
with neurocognitive deficits. Our aim was to evaluate safe, non-invasive MRI-methods
of measuring regional BBB permeability and its relationship with neurocognitive
function and regional GM volume in cSLE.
Methods:
Twelve cSLE
patients and 12 healthy controls (age, gender, race and socioeconomic status matched)
were enrolled. Those with diseases or medications (except prednisone) affecting
neurocognitive function were excluded. Cognitive performance was assessed using
the cSLE Neurocognitive Battery, which probes four
cognitive domains: working memory, psychomotor speed, attention, and visuoconstructional ability. Performance in each of these was
standardized and expressed as a Z-score. We almost concurrently performed arterial
spin labeling (ASL) and diffusion-weighted imaging to measure regional BBB
permeability. Voxel-based morphometric analysis was done to measure regional GM
volume. Voxel-wise comparisons of capillary permeability were made between the cSLE and control groups. Correlation analysis was performed
between regional BBB permeability and cognitive performance Z-scores, as well
as local GM volume for the cSLE group.
Results:
Among the cSLE patients (11 females, 7 African American, mean age 18 ± 6.8 years), 9 were treated with prednisone (median
dose 5 mg/d). None was diagnosed with active neuropsychiatric SLE. Group
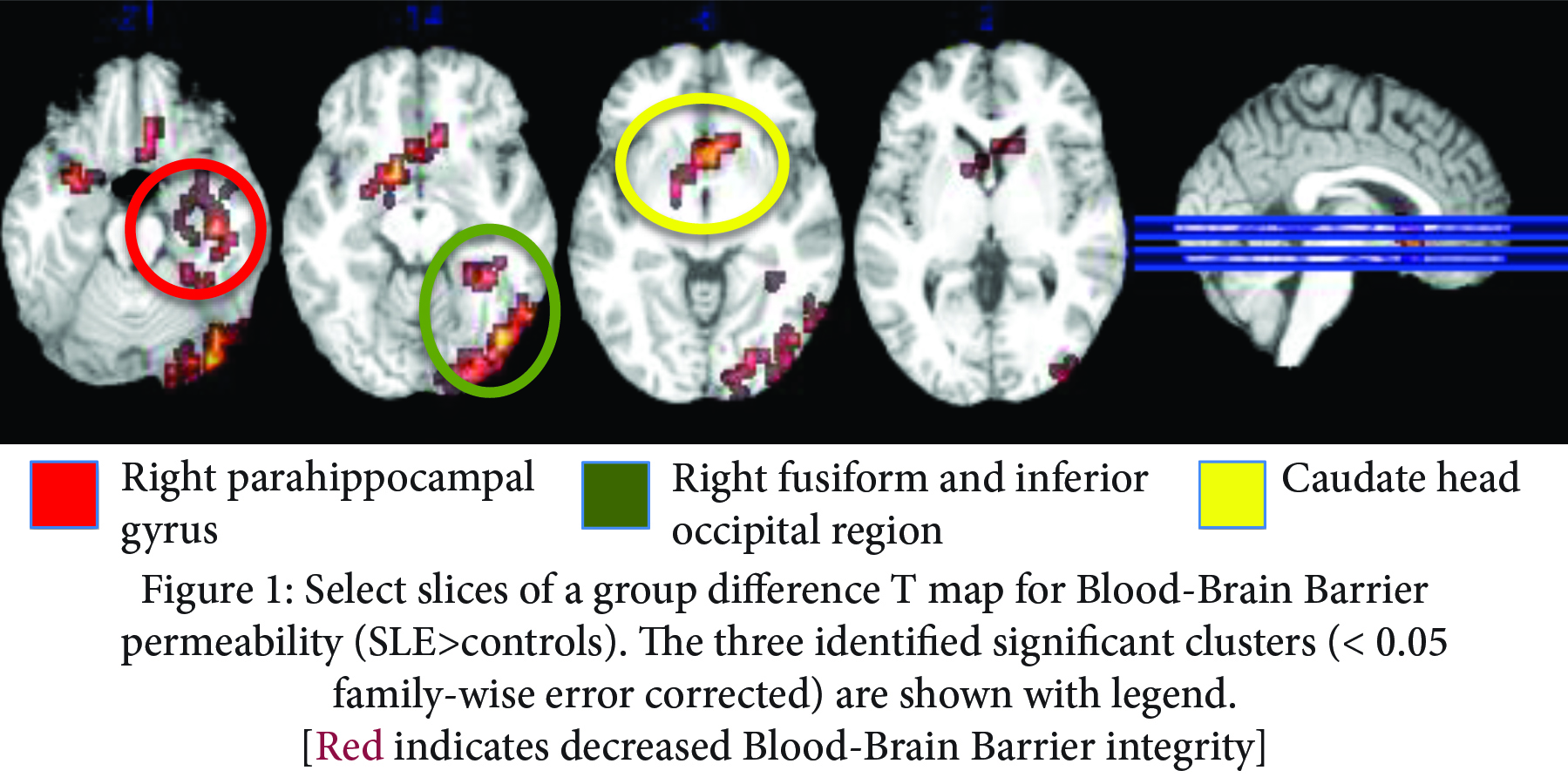
comparison revealed clusters of voxels with significantly greater BBB permeability
for cSLE patients than controls, in three regions as
shown in Figure 1. Correlations
between BBB permeability and regional GM volume or overall and individual
domain Z-scores for neurocognitive performance were not statistically
significant, although locations of significant increases in permeability for cSLE closely match our previously identified areas of GM
loss and functional changes associated with clinically overt neurocognitive
impairment.
Conclusion:
We present imaging evidence
of altered regional BBB permeability in cSLE, using a
novel non-invasive MRI technique. The absence of correlation with GM volume or cognitive
performance Z-scores, yet similar location to GM loss in previous work in our cSLE cohort suggests that BBB breakdown may precede clinically
overt neurocognitive impairment and brain tissue loss. Longitudinal studies are
needed to confirm the change in GM volume in relation to BBB permeability over
time.
To cite this abstract in AMA style:
Gulati G, Jones JT, Altaye M, Meyers Eaton J, Wiley K, DiFrancesco M, Brunner HI. Evidence of Altered Blood Brain Barrier Permeability in Systemic Lupus Erythematosus Using Magnetic Resonance Imaging [abstract]. Arthritis Rheumatol. 2015; 67 (suppl 10). https://acrabstracts.org/abstract/evidence-of-altered-blood-brain-barrier-permeability-in-systemic-lupus-erythematosus-using-magnetic-resonance-imaging/. Accessed .« Back to 2015 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/evidence-of-altered-blood-brain-barrier-permeability-in-systemic-lupus-erythematosus-using-magnetic-resonance-imaging/