Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Familial Mediterranean Fever (FMF) typically begins in childhood. It has been demonstrated that colchicine can reduce FMF attacks, prevent the development of amyloidosis, and is recommended as a lifelong treatment. Therefore, adhering to treatment is crucial.
The transition from pediatric to adult rheumatology care presents significant challenges for FMF patients diagnosed in childhood, such as moving from parental to self-care and adapting to a new clinical setting. This study aimed to assess medication adherence among FMF patients who transitioned from pediatric rheumatology to adult rheumatology care, and to identify factors that may lead to non-adherence.
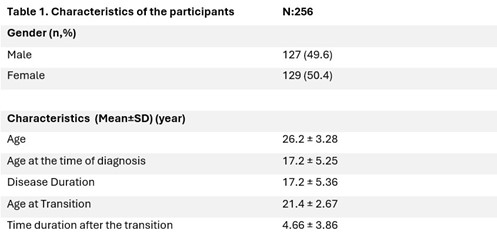
Methods: The study was conducted at the Rheumatology Clinic of Cerrahpaşa Medical Faculty between April and June 2024. It included 256 patients who were transferred from the pediatric rheumatology clinic between 2017 and 2024 and who were being treated with medications such as colchicine, anakinra, or canakinumab. The researchers noted the patients’ age, gender, age at diagnosis, age at transition, and the medications they were using during the routine examination.
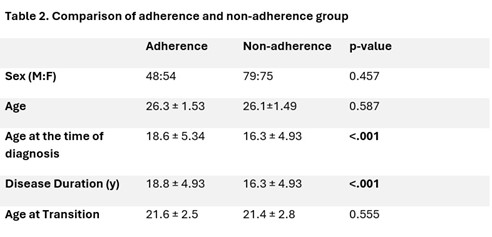
The Medication Adherence Scale in FMF (MASiF) questionnaire, consisting of 18 items, was administered to the patients. MASiF includes the items about knowledge about the medication, adherence to the treatment, barriers to drug use, factors that may increase compliance. The participants answered each item on a Likert scale (1 = strongly agree, 2 = agree, 3 = no idea, 4 = disagree, 5 = strongly disagree). 60 points and above was accepted as “adherence” and a point less than 60 was considered as “non-adherence”. Gender, age, diagnosis age, and transition age were compared between the two groups. p < 0.05 was considered significant.
Results: The patients’ characteristics are presented in Table 1. All patients were using colchicine. 21 patients (8.2%) were being treated with anakinra with colchicine, 13 patients (5%) were being treated with canakinumab in addition to colchicine. In MASiF scores, the mean was 56.9 (±10.1), the minimum was 33, the maximum was 86. 102 patients (39.6%) were considered to have medication adherence and 154 patients (60.4%) were considered to have not medication adherence. Differences between the two groups are presented in Table 2.
Conclusion: As a result, medication adherence was found to be significantly lower in patients diagnosed at a younger age and in patients with longer disease duration. Age, gender, and transition age had no significant effect on medication compliance. Our conclusions based on these results are as follows: In FMF, being diagnosed at a younger age and longer disease duration negatively affects medication compliance. Being diagnosed at a younger age may have negative effects in terms of understanding the disease, difficulty in using medication, and adequate parental support. More studies are needed on this subject. The reason for low medication compliance in patients with long disease duration may be boredom and distrust of medication. More studies are needed on this subject. Since FMF is a disease that extends from childhood to adulthood, a smooth transition period may increase adaptation.
To cite this abstract in AMA style:
Avci F, Azman F, Unsal E, Ugurlu S. Evaluation of Medication Adherence of FMF Patients Transitioned from a Pediatric Clinic to an Adult Clinic: A Cross-sectional Study [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/evaluation-of-medication-adherence-of-fmf-patients-transitioned-from-a-pediatric-clinic-to-an-adult-clinic-a-cross-sectional-study/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/evaluation-of-medication-adherence-of-fmf-patients-transitioned-from-a-pediatric-clinic-to-an-adult-clinic-a-cross-sectional-study/