Session Information
Session Type: Poster Session A
Session Time: 1:00PM-3:00PM
Background/Purpose: Interstitial pneumonia with autoimmune features (IPAF) is a subset of interstitial lung disease (ILD) which manifests with interstitial pneumonia and features of autoimmunity, yet no rheumatic disease (RD) is defined in these patients. Among other ILDs, there are robust literature that suggest specific comorbidities (ischemic heart disease, obstructive sleep apnea,lung cancer, diabetes mellitus[DM]) are associated with increased mortality. There is a paucity of studies evaluating association of comorbidities with outcomes in IPAF, specifically. The objective of this study was to evaluate the association of specific comorbidities and comorbidity burden as measured by Rheumatic Diseases Comorbidity Index (RDCI) and Charlson Comorbidity Index (CCI) with lung disease progression and mortality in IPAF.
Methods: Using a retrospective analysis study design, we evaluated the presence, type, and severity of comorbidities from manual review of the electronic medical record in a cohort of patients with IPAF at University of Texas Southwestern Medical Center. Descriptive statistics were used to express prevalence of baseline characteristics and comorbidities in patients. Using logistic regression, we correlated the presence and burden of comorbidities using CCI and RDCI with lung disease progression (defined as forced vital capacity decline of ³10%, death, or lung transplant) within two years of entry onto cohort. As a secondary outcome, we evaluated association of individual comorbidities, CCI, and RDCI with five year mortality (defined as death from any cause or lung transplant).
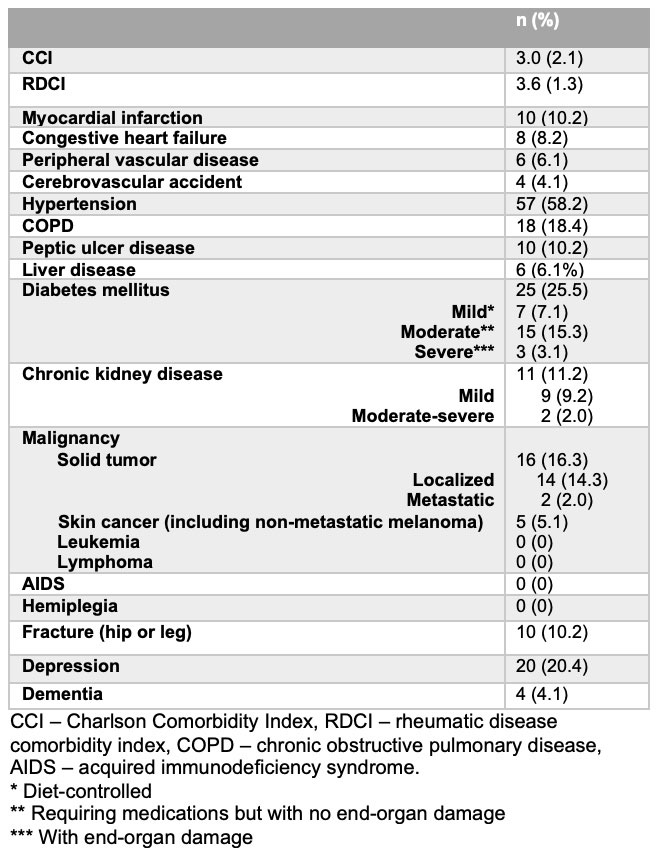
Results: A cohort of 98 patients with IPAF was created. Most prevalent comorbidities included hypertension, DM, depression, and chronic obstructive pulmonary disease (COPD). We were able to obtain primary outcome in 75 patients with IPAF. Fracture was associated with greater odds of 2-year lung disease progression (OR 6.80, 95% CI 1.52-30.50, p-value 0.012), but no other comorbidities were significantly associated with odds of progression over 2 years. Both RDCI and CCI showed a trend of higher score being associated with higher odds of 2-year progression (Table 1), with CCI being significant at significance level of 0.10. We obtained secondary outcome in 81 out of 100 patients. No baseline comorbidity, nor RDCI or CCI, were significantly associated with odds of 5-year mortality including lung transplant, although there was a trend of greater odds of mortality/lung transplant with higher RDCI and CCI.
Conclusion: Our results suggest that CCI may be a superior tool to RDCI for predicting 2-year lung disease progression in patients with IPAF. Additionally, fracture may be an important comorbidity associated with 2-year lung disease progression, suggesting the need for aggressive screening and management of this comorbidity in IPAF. Our cohort sample size was small and further larger studies are needed to validate our findings. While not statistically significant, all of the comorbidities were associated with greater odds of progression at 2 years and/or increased 5 year mortality, emphasizing the need to screen for and optimize these common comorbidities associated with IPAF.
To cite this abstract in AMA style:
Joerns E, Ghebranious M, Adams T, Makris U. Evaluation of Comorbidity Burden and Its Effect on Lung Disease Progression and Mortality in a Cohort of Patients with Interstitial Pneumonia with Autoimmune Features [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/evaluation-of-comorbidity-burden-and-its-effect-on-lung-disease-progression-and-mortality-in-a-cohort-of-patients-with-interstitial-pneumonia-with-autoimmune-features/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/evaluation-of-comorbidity-burden-and-its-effect-on-lung-disease-progression-and-mortality-in-a-cohort-of-patients-with-interstitial-pneumonia-with-autoimmune-features/