Session Information
Date: Sunday, November 12, 2023
Title: (0609–0672) Systemic Sclerosis & Related Disorders – Clinical Poster I: Research
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Gastrointestinal (GI) dysmotility affects most patients with systemic sclerosis (SSc), and the esophagus is the most commonly affected region. While most SSc patients are negatively impacted by esophageal dysmotility, significant heterogeneity exists (i.e., absent contractility, ineffective esophageal motility). Importantly prior studies demonstrate that esophageal manometry is useful for risk stratification. For example, absent contractility associates with a more severe extraintestinal clinical phenotype of SSc, (e.g., diffuse cutaneous disease, lower diffusing capacity of the lungs for carbon monoxide (DLCO) values and more severe Raynaud’s) while ineffective esophageal motility associates with a milder SSc clinical phenotype. However, manometry can be difficult to obtain due to poor access to the study, and its invasive nature limits tolerability among patient subgroups (i.e., cardiopulmonary complications). Scintigraphy offers a non-invasive alternative to manometry in characterizing motility. We therefore sought to determine (1) whether distinct SSc clinical features associate with decreased esophageal transit on scintigraphy; and (2) how such features compare to the previously described extraintestinal clinical phenotypes described in patients with absent contractility and ineffective esophageal motility on manometry.
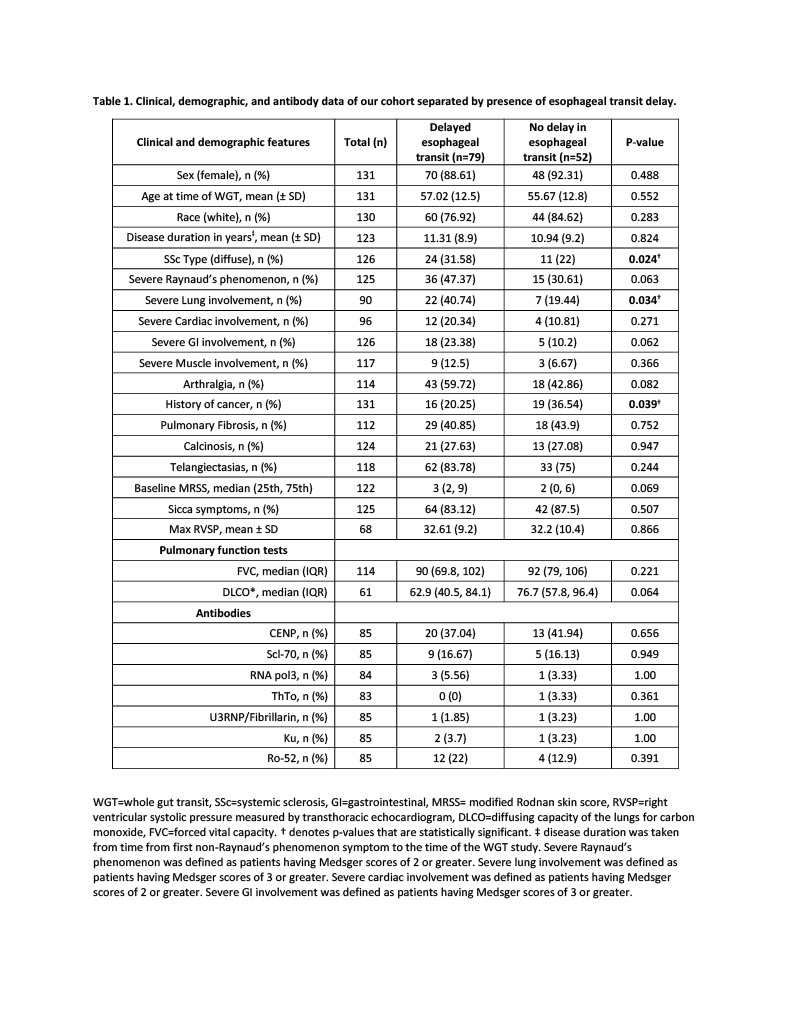
Methods: Clinical and demographic features and patient reported outcomes were compared between patients with and without delayed esophageal transit on scintigraphy. Patients were part of a prospective cohort of patients who had clinical data and blood samples collected every 6 months during clinical visits. Scintigraphy-based whole gut transit was used to measure transit time and the percent emptying in each part of the gut from the esophagus to the colon. Medsger scores were used to evaluate SSc disease activity, UCLA-GIT scores were used to evaluate GI symptoms, and the COMPASS-31 survey was used to evaluate symptoms of dysautonomia.
Results: Among 131 patients in our cohort, 79 (60%) had delayed esophageal transit and 52 (40%) did not. Patients with delayed esophageal transit were more likely to have diffuse scleroderma [24 (32%) vs. 11 (22%); p=0.024]. Esophageal transit time negatively correlated with DLCO values (correlation coefficient: -0.317; p=0.014) and % esophageal emptying at 10 seconds was positively correlated with DLCO values (correlation coefficient: 0.339; p=0.0173). Secretomotor symptoms were negatively associated with esophageal transit time (correlation coefficient -0.223; p=0.041). Interestingly, patients with delayed esophageal transit had a higher median (IQR) diarrhea GIT score [0.5 (0-1) vs. 0 (0-1); p=0.050].
Conclusion: Our results suggest that esophageal scintigraphy is a useful tool that can identify patients with a more severe SSc phenotype. Furthermore, patients with delayed esophageal transit on scintigraphy have similar clinical characteristics to SSc patients with absent contractility diagnosed on manometry. Further studies are needed to determine whether esophageal scintigraphy may serve as non-invasive tool to identify SSc patients who may have specific GI and extraintestinal complications.
To cite this abstract in AMA style:
Salas A, Yanek L, McMahan Z. Evaluating Esophageal Dysmotility by Scintigraphy in Systemic Sclerosis: Subsets and Phenotypes [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/evaluating-esophageal-dysmotility-by-scintigraphy-in-systemic-sclerosis-subsets-and-phenotypes/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/evaluating-esophageal-dysmotility-by-scintigraphy-in-systemic-sclerosis-subsets-and-phenotypes/