Session Information
Date: Monday, October 27, 2025
Title: (1553–1591) Systemic Sclerosis & Related Disorders – Clinical Poster II
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: The inpatient epidemiology, morbidity, mortality, and healthcare expenditures of patients with systemic sclerosis (SSc) are not well-characterized. This study aims to utilize a nationwide inpatient database to better describe these parameters.
Methods: Patients with SSc were identified in the 2021 Nationwide Inpatient Sample (NIS) using ICD-10-CM codes. The NIS is the largest all-payer inpatient database in the United States, encompassing data from over 4,000 non-federal acute care hospitals, and is representative of all U.S. acute care hospitalizations. A comparison cohort without SSc was created for comparative analysis. Extracted data included demographics, primary admission diagnoses, length of stay, mortality, morbidity, expenditures, and comorbidities. Comparative analyses were adjusted for age, sex, ethnicity, Charlson Comorbidity Index, payer type, income, and hospital characteristics.
Results: The inpatient prevalence of SSc was 86.7 per 100,000 admissions. The most common primary admission diagnoses among SSc patients were sepsis (22.7%), hypertension with heart failure (14.4%), and COVID-19 infection (11.5%). The SSc cohort was predominantly female (84.2%) with a mean age of 63.5 years. Compared with non-SSc hospitalizations, those with SSc had significantly longer hospital stays (by 0.7 days; 95% CI: 0.5–0.9) and higher costs, including an adjusted mean increase of $3,277 (95% CI: $2,051–$4,504) in total hospital costs and $11,801 (95% CI: $6,485–$17,116) in total hospitalization charges. Patients with SSc also experienced worse outcomes, including higher risk of in-hospital mortality (adjusted OR 1.42; 95% CI: 1.26–1.61), shock (OR 1.30; 95% CI: 1.17–1.44), systemic inflammatory response syndrome (OR 1.32; 95% CI: 1.01–1.74), and acute respiratory distress syndrome (OR 1.45; 95% CI: 1.12–1.87). Additionally, hospitalized SSc patients had a higher prevalence of multiple comorbidities compared to the control group (see Table 1).
Conclusion: The inpatient prevalence of SSc is substantially higher than its prevalence in the general population, suggesting that individuals with SSc require inpatient care more frequently. SSc hospitalizations are associated with poorer clinical outcomes and significantly higher healthcare expenditures.
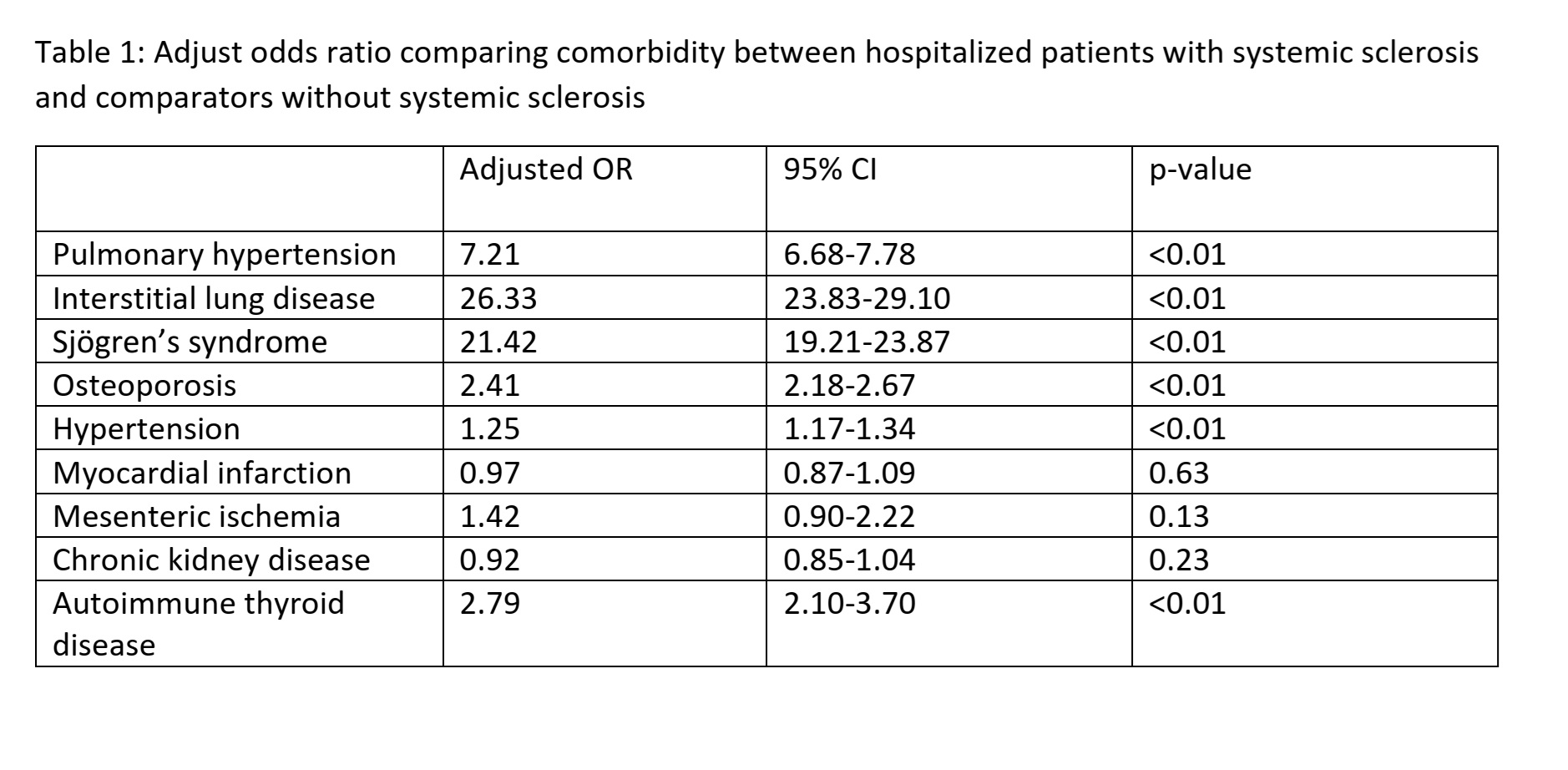 Table 1: Adjust odds ratio comparing comorbidity between hospitalized patients with systemic sclerosis and comparators without systemic sclerosis
Table 1: Adjust odds ratio comparing comorbidity between hospitalized patients with systemic sclerosis and comparators without systemic sclerosis
To cite this abstract in AMA style:
Ungprasert P, Kroner P. Epidemiology, Outcome and Expenditures of Hospitalized Patients with Systemic Sclerosis: National Inpatient Sample 2021 [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/epidemiology-outcome-and-expenditures-of-hospitalized-patients-with-systemic-sclerosis-national-inpatient-sample-2021/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/epidemiology-outcome-and-expenditures-of-hospitalized-patients-with-systemic-sclerosis-national-inpatient-sample-2021/
