Session Information
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: During the course of hospitalization, it is often unclear which COVID-19 patients will progress from non-critical to critical illness. Timely identification of these patients is crucial to guiding triage and early immunomodulatory intervention. Biomarkers linked with inflammation, such as CRP, D-dimer, ferritin, and procalcitonin are associated with critical illness or mortality in COVID-19 infection. These laboratory values are of particular interest due to their correlation with pathologic mechanisms related to IL-1 and IL-6 signaling as well as coagulopathy. We sought to determine whether these markers could be predictive in assessing whether a patient with non-critical illness would progress to critical disease.
Methods: In our single-center retrospective cohort analysis of the first 66 patients admitted for COVID-19 infection, we examined inflammation biomarkers to distinguish non-critically ill inpatients who remained stable from those that had progressive respiratory failure requiring intubation and ICU transfer. Unlike the typical approach where patients are grouped into the two categories of non-critical and critical illness, COVID-19 patients in our study were classified into three cohorts by severity and stability of respiratory failure: stable non-critical illness (“mild”, 38 [58%]); non-critical illness at admission that progressed to critical illness (“progressive”, 21 [32%]); and critical illness at admission (“severe”, 7 [11%]). This approach allowed us independently profile patients with progressive disease from those who were already critically ill on admission.
Results: We found that while admission CRP level was weakly associated with future progressive respiratory failure, it had limited clinical utility as the progressive cohort showed modestly increased levels of CRP compared to the mild cohort, with significant overlap (125.0 ± 74 vs. 81.3 ± 57 mg/L, P = 0.05) (Figure 1). Despite the limited predictive value of admission CRP levels, these measurements were indeed clinically relevant as they correlated with SOFA score (ρ = 0.41, P < 0.001) and hypoxemic respiratory failure (PaO2/FiO2, r = -0.58, P < 0.001) (Figure 2). A closer examination of CRP trend showed that dynamic trend of CRP levels within the first 72 hours of admission rather than the static CRP level at admission showed a much stronger association with respiratory deterioration. Specifically, rise in CRP levels most clearly distinguished mild and progressive cohorts (24-48h post-admission: 170.6 ± 95 vs. 91.0 ± 67 mg/L, P = 0.03; 48-72h post-admission: 185.0 ± 92 vs. 81.6 ± 63 mg/L, P = 0.002) (Figure 3).
Conclusion: Closely tracking the CRP levels in the hyper-acute phase of admission for COVID-19 patients was predictive of progression to critical illness, suggesting that trends of inflammatory biomarkers, rather than absolute admission values, may have most utility for clinical triage and targeting therapeutic immunomodulation. Moreover, separating out patients with progressive disease identified a unique biomarker phenotype, indicating that clinical trials of anti-IL6 receptor monoclonal antibodies should pay parti
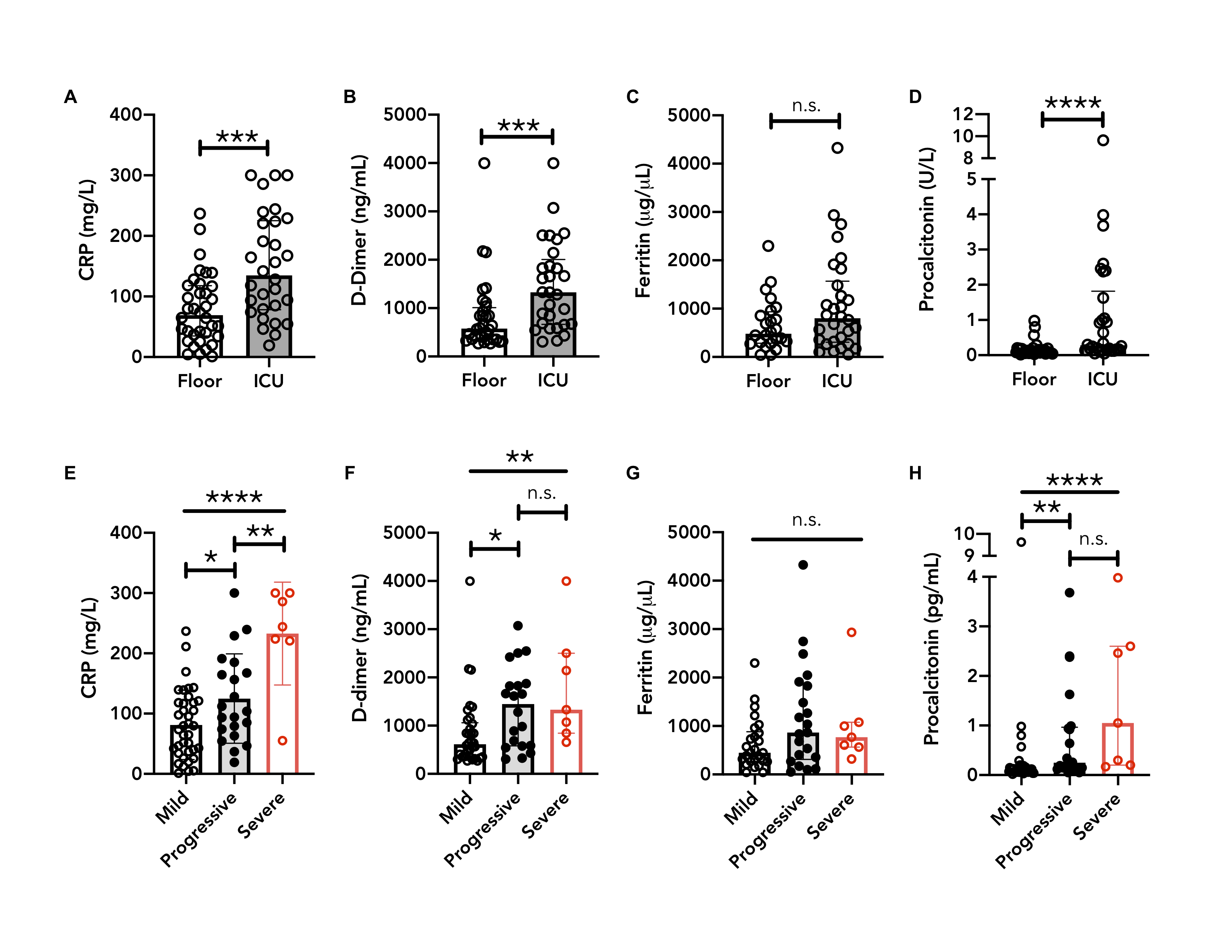 Admission CRP and D-dimer values associate with mild, progressive and severe respiratory failure. A-D: Initial levels of A) CRP; B) D-dimer; C) Ferritin; D) Procalcitonin are shown for patients with non-critical illness (“Floor”; n = 36) or with critical illness (“ICU”; n = 30). E-H: Patients grouped into “mild” (stable, non-critical respiratory failure; n = 38), “progressive” (initial non-critical respiratory failure that progressed to intubation during admission; n = 21), and “severe” (intubation on day of admission; n = 7) cohorts. Initial levels of E) CRP, F) D-dimer, G) Ferritin, and H) Procalcitonin are shown. Mann-Whitney U test performed for A-G. ANOVA and Tukey’s multiple comparison performed for H. *P < 0.05, **P < 0.01, ***P < 0.001, ****P < 0.0001. Kruskal-Wallis test with Dunn’s multiple comparison used for E-H. CRP, C-reactive protein; n.s., non-significant.
Admission CRP and D-dimer values associate with mild, progressive and severe respiratory failure. A-D: Initial levels of A) CRP; B) D-dimer; C) Ferritin; D) Procalcitonin are shown for patients with non-critical illness (“Floor”; n = 36) or with critical illness (“ICU”; n = 30). E-H: Patients grouped into “mild” (stable, non-critical respiratory failure; n = 38), “progressive” (initial non-critical respiratory failure that progressed to intubation during admission; n = 21), and “severe” (intubation on day of admission; n = 7) cohorts. Initial levels of E) CRP, F) D-dimer, G) Ferritin, and H) Procalcitonin are shown. Mann-Whitney U test performed for A-G. ANOVA and Tukey’s multiple comparison performed for H. *P < 0.05, **P < 0.01, ***P < 0.001, ****P < 0.0001. Kruskal-Wallis test with Dunn’s multiple comparison used for E-H. CRP, C-reactive protein; n.s., non-significant.
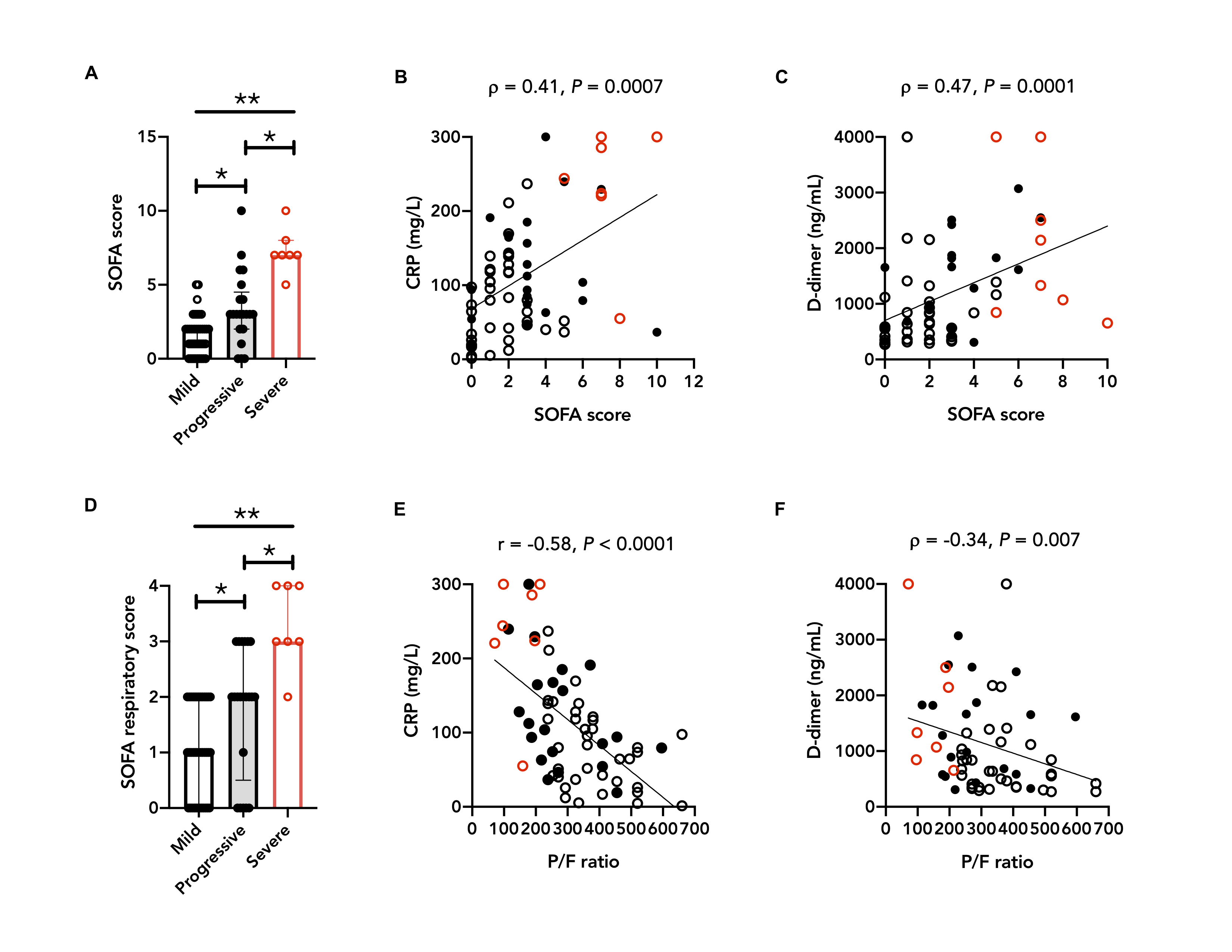 Admission CRP values associate with SOFA score and PaO2/FiO2 (P/F) ratio. COVID-19 inpatients are grouped into mild, progressive or severe cohorts defined by respiratory failure. A) SOFA scores on admission. B-C: Correlation of SOFA scores to initial B) CRP; C) D-dimer. D) SOFA respiratory scores on admission. E-F: Correlation of P/F ratios to initial E) CRP; F) D-dimer. Open black circles, mild; filled black circles, progressive; open red circles, severe. Kruskal-Wallis test and Dunn’s multiple test were performed for A and D; Spearman rank correlation for B, C, and F; Pearson correlation for E. *P < 0.05, **P < 0.01. CRP, C-reactive protein; P/F, PaO2/FiO2; SOFA, Sequential Organ Failure Assessment.
Admission CRP values associate with SOFA score and PaO2/FiO2 (P/F) ratio. COVID-19 inpatients are grouped into mild, progressive or severe cohorts defined by respiratory failure. A) SOFA scores on admission. B-C: Correlation of SOFA scores to initial B) CRP; C) D-dimer. D) SOFA respiratory scores on admission. E-F: Correlation of P/F ratios to initial E) CRP; F) D-dimer. Open black circles, mild; filled black circles, progressive; open red circles, severe. Kruskal-Wallis test and Dunn’s multiple test were performed for A and D; Spearman rank correlation for B, C, and F; Pearson correlation for E. *P < 0.05, **P < 0.01. CRP, C-reactive protein; P/F, PaO2/FiO2; SOFA, Sequential Organ Failure Assessment.
 Hyper-acute CRP trend distinguishes stable and progressive respiratory failure. COVID-19 inpatients are grouped into mild, progressive or severe cohorts defined by respiratory failure. A-B: Maximum values during hospital course are shown for A) CRP; B) ferritin. C-D: Mean CRP values are shown as a function of C) days after first recorded CRP level; D) days after onset of first symptom. E) CRP values for patients with mild or progressive disease taken 0-24, 24-48, and 48-72 hours after admission. A-B, median and interquartile range are plotted; C-E, mean and standard deviation are plotted. Open black circles, mild; filled black circles, progressive; open red circles, severe. Kruskal-Wallis test and Dunn’s multiple test were performed for A and B; a mixed effect model was used for E. *P < 0.05, **P < 0.01, ***P < 0.001. CRP, C-reactive protein; Max, maximum; n.s., non-significant.
Hyper-acute CRP trend distinguishes stable and progressive respiratory failure. COVID-19 inpatients are grouped into mild, progressive or severe cohorts defined by respiratory failure. A-B: Maximum values during hospital course are shown for A) CRP; B) ferritin. C-D: Mean CRP values are shown as a function of C) days after first recorded CRP level; D) days after onset of first symptom. E) CRP values for patients with mild or progressive disease taken 0-24, 24-48, and 48-72 hours after admission. A-B, median and interquartile range are plotted; C-E, mean and standard deviation are plotted. Open black circles, mild; filled black circles, progressive; open red circles, severe. Kruskal-Wallis test and Dunn’s multiple test were performed for A and B; a mixed effect model was used for E. *P < 0.05, **P < 0.01, ***P < 0.001. CRP, C-reactive protein; Max, maximum; n.s., non-significant.
To cite this abstract in AMA style:
Mueller A, Tamura T, Jezmir J, Penn E, Keras G, Massaro A, Kim E. Early Rise in CRP Is Associated with Progression to Respiratory Failure and Intubation in COVID-19 Patients [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/early-rise-in-crp-is-associated-with-progression-to-respiratory-failure-and-intubation-in-covid-19-patients/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/early-rise-in-crp-is-associated-with-progression-to-respiratory-failure-and-intubation-in-covid-19-patients/
