Session Information
Session Type: Poster Session D
Session Time: 9:00AM-11:00AM
Background/Purpose: Individuals with knee osteoarthritis (OA) are increasingly living with multiple comorbid conditions. The presence of comorbidities has been associated with having worse OA symptoms but few studies have assessed their impact on response to OA treatment. We assessed the impact if any of comorbidities on improvement in pain and physical function (patient-reported and performance-based) in recipients of total knee arthroplasty (TKA) for knee OA.
Methods: In the BEST Knee prospective cohort study, patients with knee OA underwent assessment one month prior and 12 months after TKA at two tertiary referral centres in Alberta Canada. Standardized questionnaires assessed sociodemographics social support smoking status self-reported comorbidities and patient-reported outcomes (WOMAC pain, KOOS physical function short-form). Using multivariable generalized-estimating-equation extension of linear regression accounting for potential clustering by surgeon and adjusting for potential confounders we assessed the impact of specific comorbid conditions a priori hypothesized to impact pain and function and total number of conditions reflective of total comorbidity burden separately on change in patient-reported knee pain and physical function at 12 months after TKA. In an exploratory analysis in a subset of patients for whom six-minute walk test (6MWT) a performance-based measure of functional exercise capacity was performed one month prior and 12 months after TKA we assessed the impact of specific and total number of comorbid conditions on change in walking distance.
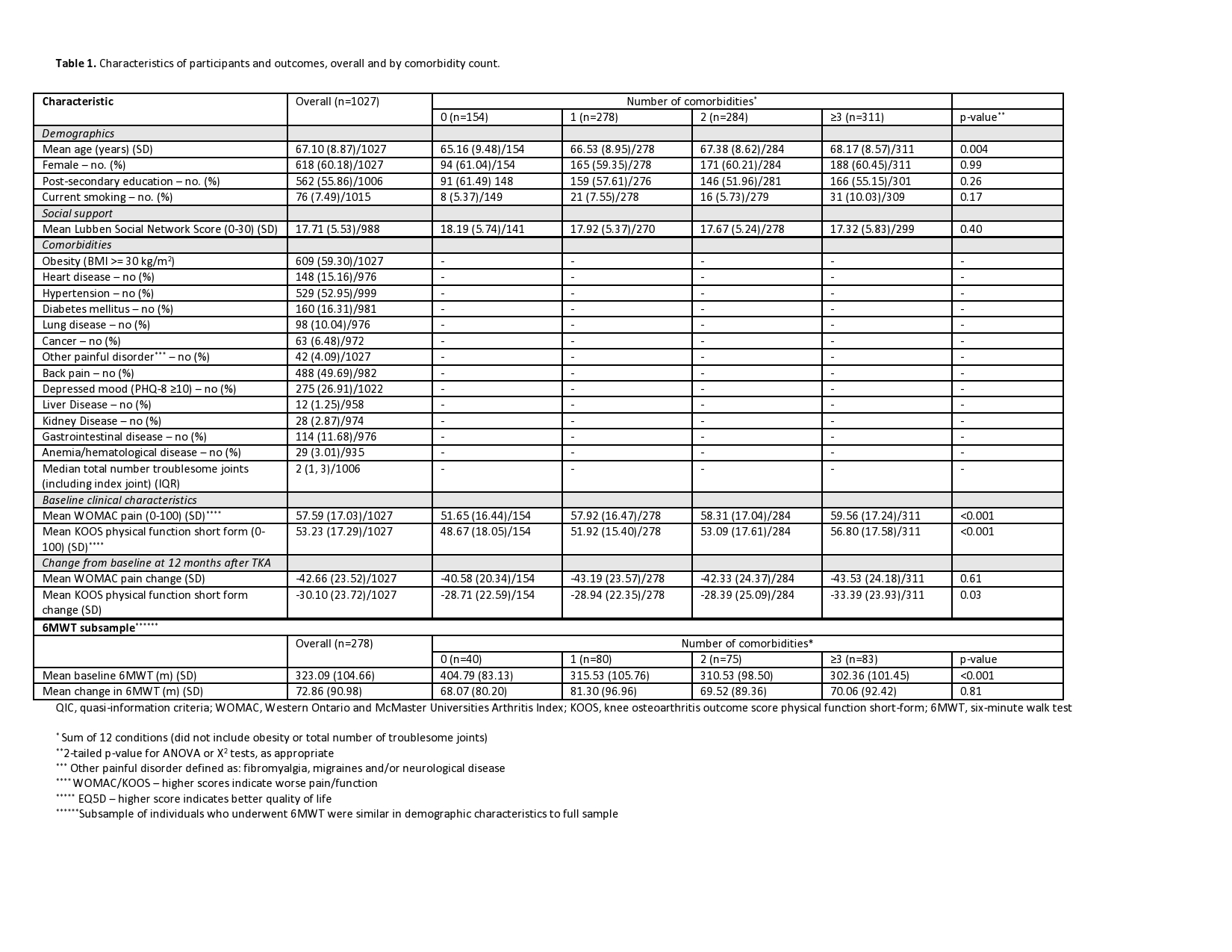
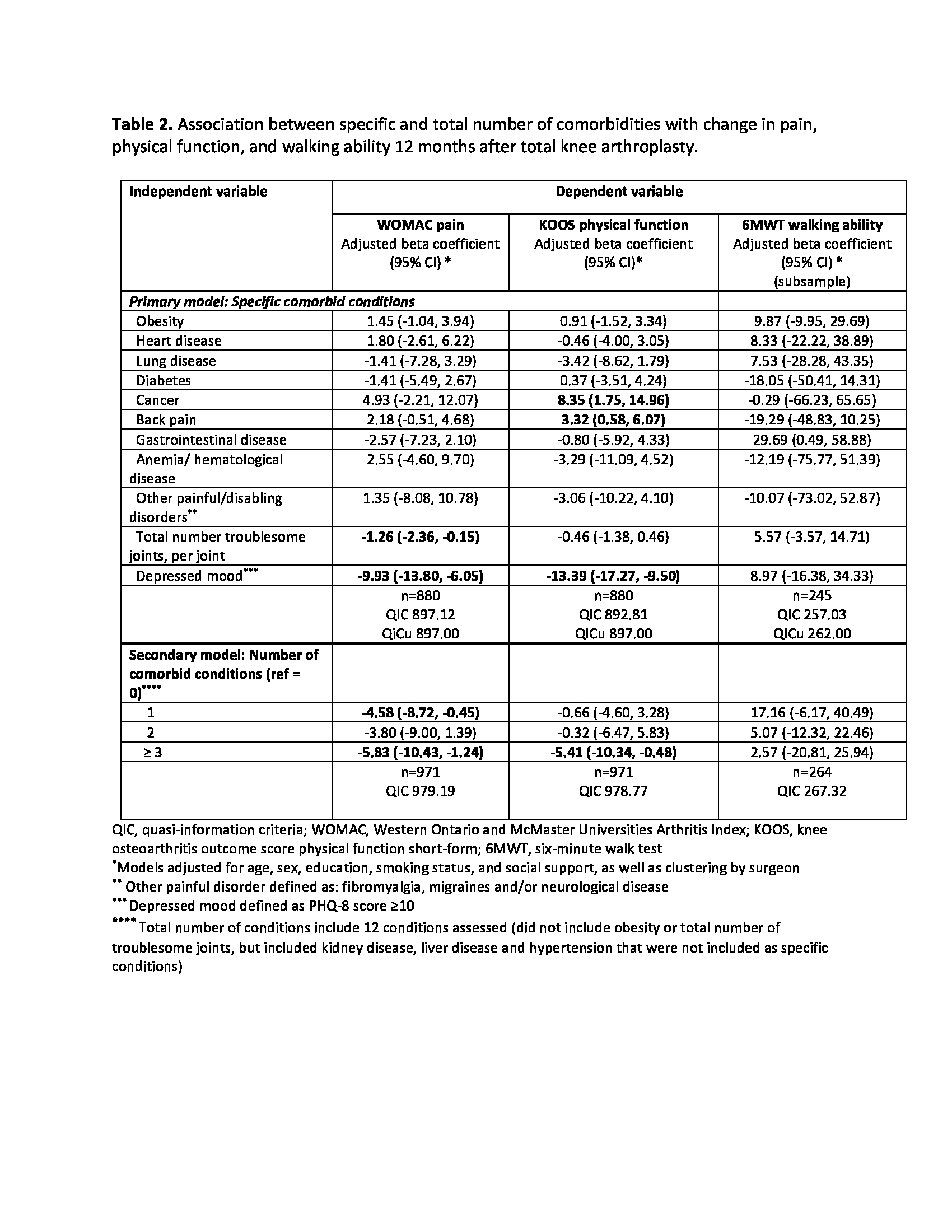
Results: 1027 participants were included (Table 1) 278 for the 6MWT subset. Mean age was 67 years (SD 8.87) 60% were female 59.3% had a BMI ≥ 30 kg/m2 and 85% reported at least one comorbidity. Individuals with higher number of comorbidities had worse pre-TKA scores for pain physical function and walking distance. At follow-up mean changes in pain function and walking distance were similar for those with and without comorbidities (Table 1). In regression analysis back pain (ß=3.3, 95% CI: 0.6 to 6.1) and cancer (ß=8.4, 95% CI 1.8 to 15.0) were associated with less improvement in patient-reported physical function while depressed mood and a higher total number of conditions were associated with greater improvement in both pain and function. No specific conditions were associated with less improvement in pain. Improvement in walking distance after TKA as measured by the 6MWT was unrelated to specific and total number of conditions (Table 2).
Conclusion: For individuals with knee OA most comorbid conditions do not limit improvement in pain physical function and walking distance (6MWT) after TKA. Understanding response to OA treatment in individuals with comorbidities is important for individualized patient counselling. For patients living with comorbidities these findings are important as improvement in long-term OA outcomes may facilitate better engagement in self-management such as physical activity for their other conditions.
To cite this abstract in AMA style:
King L, Waugh E, Jones A, Marshall D, Hawker G. Do Comorbidities Limit Improvement in Pain and Physical Function After Total Knee Arthroplasty in Patients with Knee Osteoarthritis? [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/do-comorbidities-limit-improvement-in-pain-and-physical-function-after-total-knee-arthroplasty-in-patients-with-knee-osteoarthritis/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/do-comorbidities-limit-improvement-in-pain-and-physical-function-after-total-knee-arthroplasty-in-patients-with-knee-osteoarthritis/