Session Information
Date: Sunday, October 26, 2025
Title: (0671–0710) Systemic Sclerosis & Related Disorders – Clinical Poster I
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Pulmonary arterial hypertension (PAH) is a severe complication of systemic sclerosis (SSc), associated with high morbidity and mortality. Accurate and early diagnosis of SSc-PAH is essential to initiate targeted therapies that may improve outcomes by counteracting key pathophysiological mechanisms. Breathomics, the analysis of volatile organic compounds (VOCs) in exhaled breath, has emerged as a promising non-invasive tool, as VOCs reflect underlying metabolic and pathological processes. This study investigates the potential of breathomics in SSc-PAH, both for disease understanding and diagnosis.
Methods: fourteen SSc patients with a diagnosis of PAH confirmed by right heart catheterization, 28 age- and sex-matched SSc patients without PAH, and 36 matched healthy controls (HCs)were enrolled in a single-center, case-control observational study. Exhaled breath VOCs were collected using the ReCIVA® breath sampler connected to a clean air supply (CASPER®). Samples were trapped on sorbent tubes and analyzed by thermal desorption gas chromatography–mass spectrometry (TD-GC-MS) at Owlstone Medical. VOCs were chemically identified according to Metabolomics Standards Initiative (MSI) criteria, and blank air samples were analyzed to distinguish true breath compounds from environmental contaminants. Data were analyzed using linear regression, adjusting for relevant covariates and excluding outliers.
Results: all SSc participants were female and predominantly affected by lcSSc (n = 23, 63.4%) and mostly tested positive for ACA (n = 40, 85%). The mean age was 68 ± 9 years, with no differences between the SSc-PAH and SSc-noPAH groups. A total of 1.382 VOCs were analyzed; of these, 186 were confirmed to be genuinely present “on breath” and annotated with high confidence (MSI tier 1 or 2). Among these, 55 VOCs significantly differentiated SSc-PAH from SSc-noPAH, and 40 differentiated SSc-PAH from healthy controls. Notably, 32 VOCs distinguished SSc-PAH from both comparator groups (p < 0.05 and |fold change| > 1.5) (Figure 1). Findings of interest included: a reduction in terpenes in SSc-PAH, potentially reflecting impaired vasodilatory capacity (Figure 2); a decrease in sulfur-containing compounds, suggestive of reduced control over vasoconstriction; a reduction end-products (i.e. 1-pentene) of allyl organosulfur derivates with anti-inflammatory properties; an increase in pyrazines, possibly indicative of enhanced gut permeability; and elevated levels of the uremic toxin m-cresol, which has been associated with endothelial dysfunction.
Conclusion: breathomics revealed a distinct metabolic signature in SSc-PAH, distinguishing it from both SSc without PAH and healthy controls. The identified VOCs not only hold promise as non-invasive biomarkers for early diagnosis but also shed light on key pathogenic mechanisms of PAH, including impaired vasoregulation, increased gut permeability, and endothelial dysfunction. These findings support the role of breath analysis as a valuable tool for both clinical and mechanistic insights in SSc-PAH.
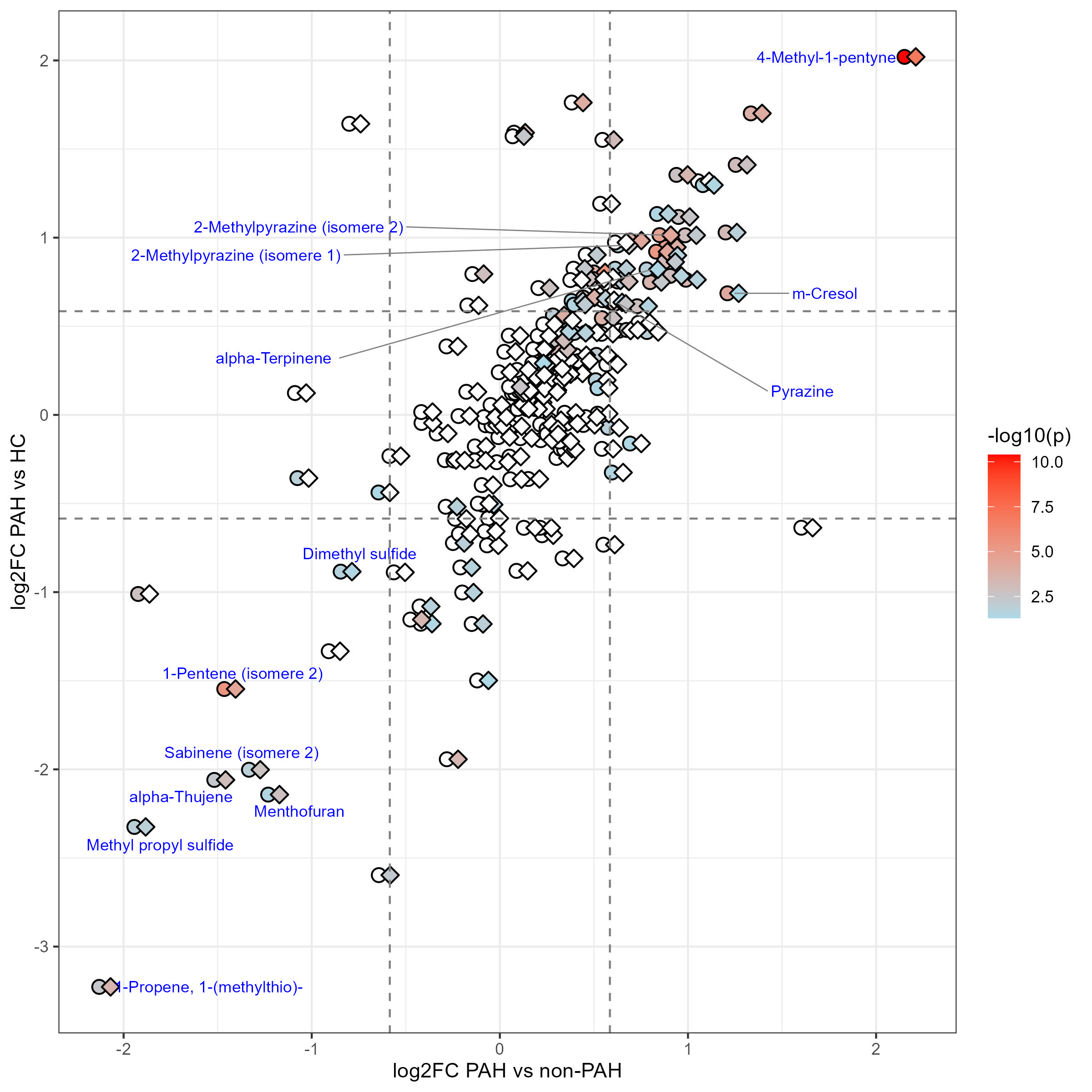 Figure 1 – Pairwise logFC comparison of SSc-PAH vs comparators
Figure 1 – Pairwise logFC comparison of SSc-PAH vs comparators
.jpg) Figure 2 – Principal component analysis biplot of terpenes across study groups
Figure 2 – Principal component analysis biplot of terpenes across study groups
To cite this abstract in AMA style:
Iacubino M, Rocco L, Vicenzi M, Bellocchi C, Mozzo M, severino a, Caronni M, Santaniello A, montanelli G, Vigone B, Grimmett L, Kerr M, Beretta L. Distinct Breath Metabolomic Signature in Systemic Sclerosis Patients with Pulmonary Arterial Hypertension [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/distinct-breath-metabolomic-signature-in-systemic-sclerosis-patients-with-pulmonary-arterial-hypertension/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/distinct-breath-metabolomic-signature-in-systemic-sclerosis-patients-with-pulmonary-arterial-hypertension/
