Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: The prevalence of comorbidities is increased in patients with rheumatoid arthritis (RA) compared to the general population1, but their impact in the earlier stages of the disease and potential sex differences are much less known.
Our aim was to analyze the influence of comorbidities on the clinical evolution of patients from an Early Arthritis Clinic (EAC) and to explore sex differences to identify potential gender biases.
Methods: Patients attended between September 2001 and December 2021 in an EAC of a tertiary hospital were studied. Sociodemographic, clinical, and therapeutic variables were collected prospectively during protocolized visits (baseline, 6, 12, and 24 months). Information on the presence and date of diagnosis of comorbidities was obtained retrospectively by reviewing hospital and primary care medical records. Only comorbidities detected prior to baseline visit and those diagnosed within the 2 years of follow-up were considered. The statistical analysis was performed using Stata 14.1 with appropriate tests for bivariate analysis based on the type and distribution of the variables. To analyze the influence of comorbidities (considered as a categorical variable: none, 1, 2 or ≥3) on disease activity (HUPI)² and disability (HAQ), two multivariable models nested by patient and visit were fitted using the command xtgee. All variables with p< 0.15 in the bivariate analysis were included in the initial models and then independent variables were excluded if p >0.15.
Results: We studied 556 patients (443 women, 80%). Women were significantly younger at disease onset (53 years [IQR 42 – 64] vs 63 [IQR 51 – 71], p< 0.001), with no significant differences in positivity for rheumatoid factor (54.1%) or ACPA (50.5%) by sex. At 2 years, 71% of the patients met the criteria for RA (ACR/EULAR 2010), while 29% remained as undifferentiated arthritis, with a similar distribution by sex.
Men had higher frequencies of arterial hypertension (47.79% vs 21.44% in women; p< 0.001), diabetes mellitus (18.58% vs 6.32%; p< 0.001), ischemic heart disease (10.62% vs 1.81%; p< 0.001), COPD (9.73% vs 1.58%; p < 0.001), and peptic ulcer (3.54% vs 0.68%; p=0.015); while women had higher frequencies of depression (19.19% vs 8.85% in men; p=0.009) and osteoporosis (23.70% vs 11.50%; p=0.005).
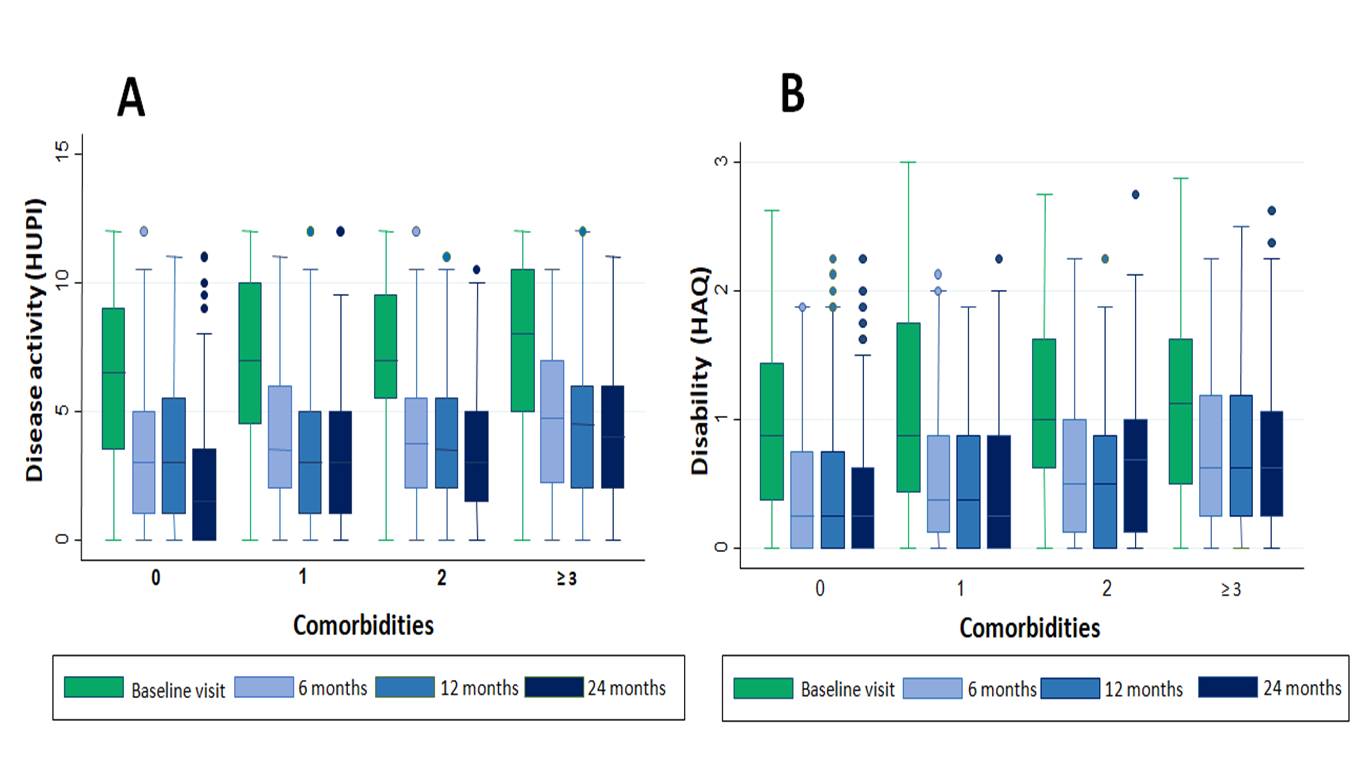
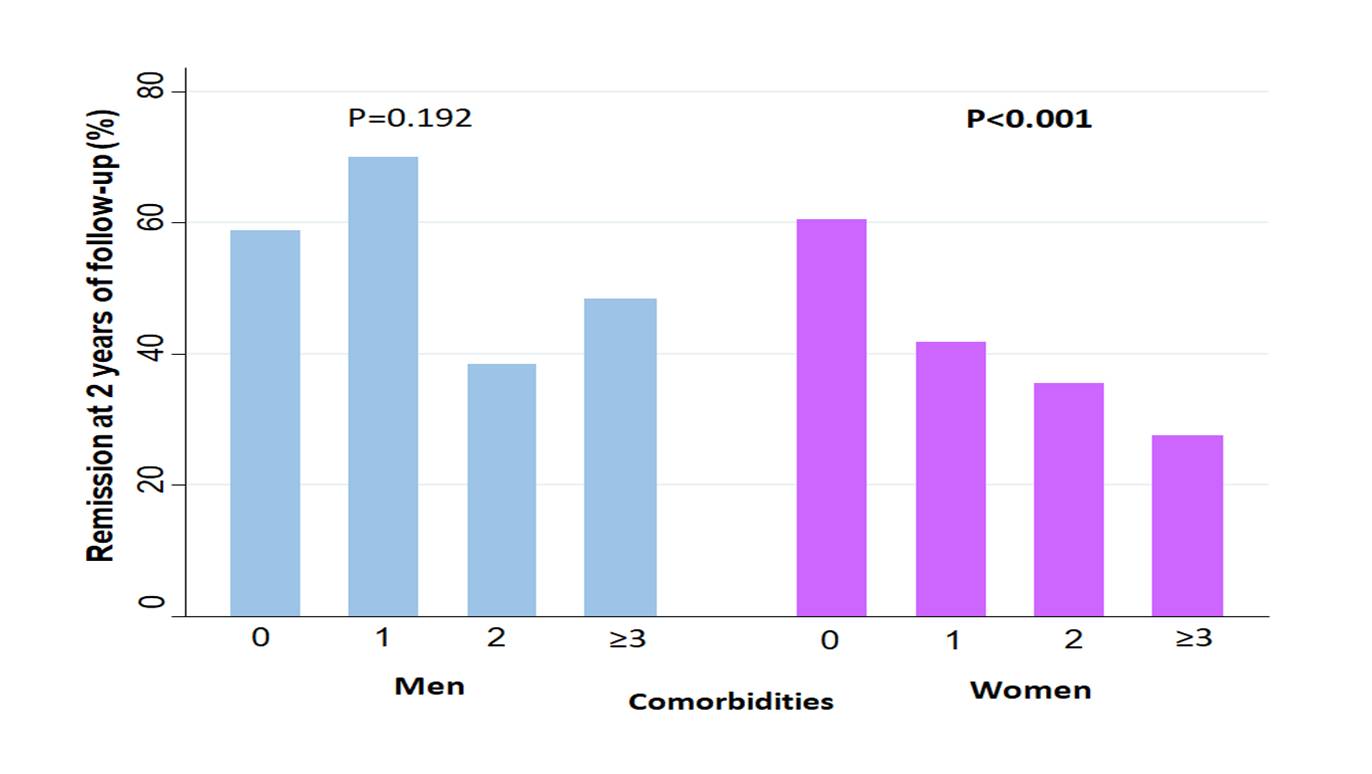
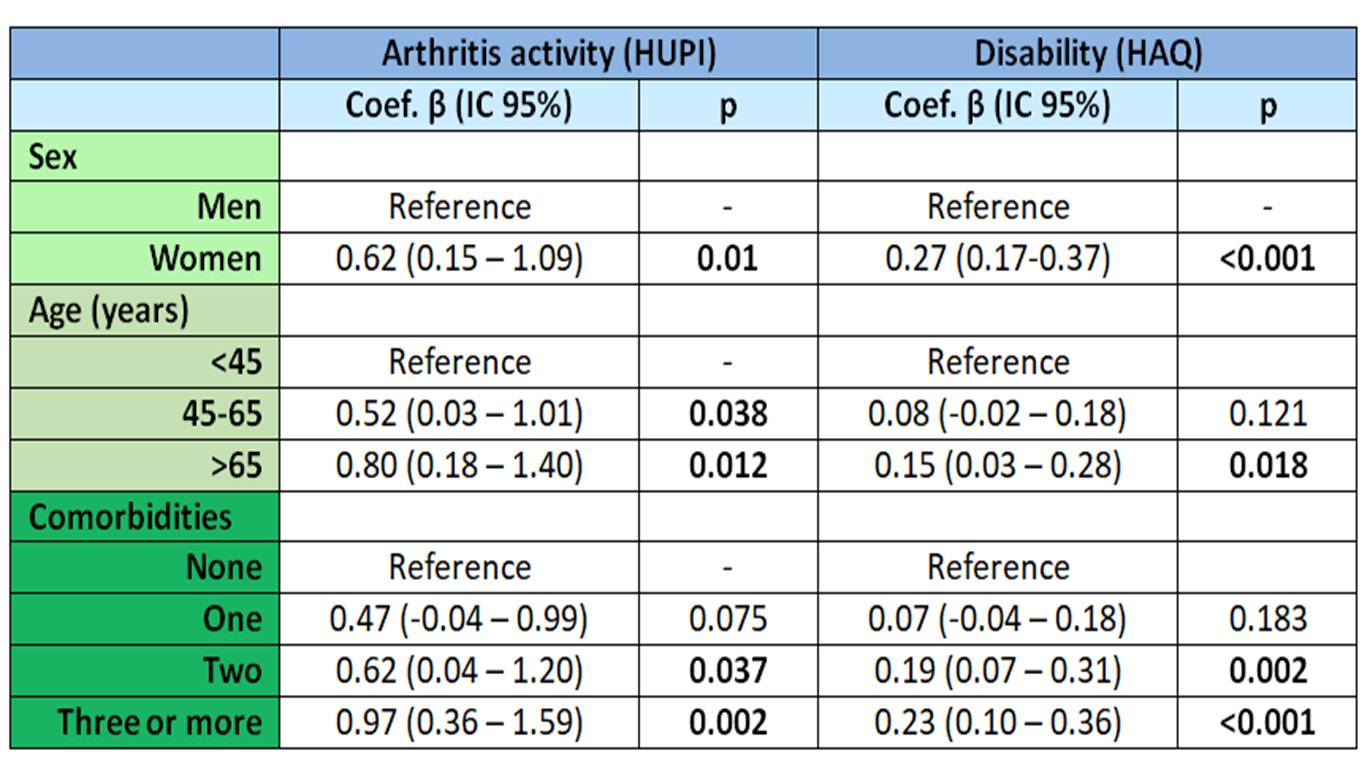
As observed in Figure 1, the disease activity evolution (1A) and disability (1B) worsened with a higher number of comorbidities. Multivariable analysis showed that older age and female sex were significantly associated with higher disease activity and disability, Adjusted for these variables, the presence of a greater number of comorbidities was also associated with worse outcomes (Table 1). However, frequency of remission (HUPI < 2)² at 2 years of follow-up was significantly lower with increasing number of comorbidities only in women (Figure 2).
Conclusion: The presence of comorbidities influences a worse progression in both disease activity and disability, with a more pronounced effect observed in women.
1. Carmona L et al. Best Pract Res Clin Rheumatol. 2010; 24(6):733-45.
2. González Alvaro et al. PLos One, 2016; 11(9):e0161727.
To cite this abstract in AMA style:
Dueñas M, Sáez J, Álvarez M, Quiroga P, Nikitsina M, García-Vicuña R, Ortiz A, González-Álvaro I, Llorente-Cubas I. Differential Effect of Comorbidities on the Clinical Evolution of Early Arthritis by Sex [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/differential-effect-of-comorbidities-on-the-clinical-evolution-of-early-arthritis-by-sex/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/differential-effect-of-comorbidities-on-the-clinical-evolution-of-early-arthritis-by-sex/