Session Information
Date: Saturday, November 16, 2024
Title: Abstracts: Pain in Rheumatic Disease Including Fibromyalgia
Session Type: Abstract Session
Session Time: 1:00PM-2:30PM
Background/Purpose: England has seen a notable rise in prescription opioid use over the past two decades, leading to some of Europe’s highest opioid-related hospital admissions. Patients with Rheumatic and Musculoskeletal Diseases (RMDs) are especially at risk due to multimorbidity and long-term opioid use. Machine learning-based clinical prediction models (CPMs) could improve risk assessment in this context by addressing nonlinear relationships. We aimed to develop and evaluate CPMs based on regression and ML, using nationally representative UK data, to estimate the risk of opioid-related hospitalizations in RMD patients for non-cancer pain.
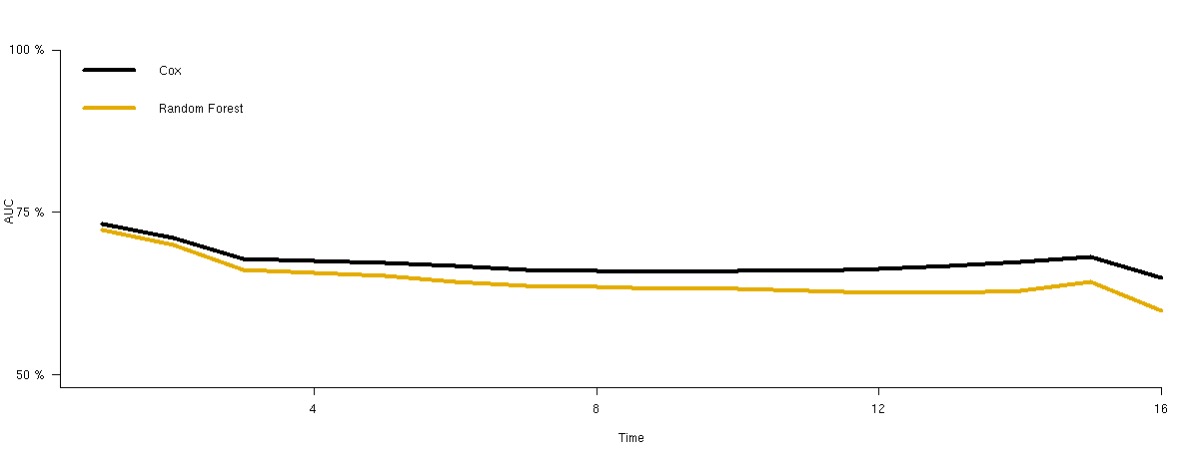
Methods: We conducted a retrospective cohort study using the Clinical Research Practice Datalink, a large UK primary care electronic health record database, from 2006-2021. Patients included were new opioid users aged ≥18 years old with one or more RMDs (osteoarthritis, fibromyalgia, rheumatoid arthritis, axial spondyloarthritis, systemic lupus erythematosus, or psoriatic arthritis). Patients with a history of cancer were excluded. Opioid-related hospital admissions (any admission code including opioid poisoning, fractures, falls, delirium, sleep disorders and constipation) were identified using Hospital Episode Statistics Admitted Patient Care and Accident and Emergency Attendances. Candidate predictors were selected based on clinical relevance from prior literature. Patients were considered ‘at risk’ from their first new opioid prescription and were censored at first admission, death, loss of follow-up or after two years without opioid prescription. CPMs using Cox proportional hazards (CPH) and Random Survival Forest were trained with time-to-event patient data. Predictive performance was evaluated by calculating the area under the receiver characteristic operator curve (AUC) using 5-fold cross validation.
Results: Over a 15-year period, 1,070,719 unique patients (59.5% female, median age [IQR]: 62 [25]) were new opioid users diagnosed with one or more RMDs. Opioid-related hospitalization occurred in 43,728 patients (4.1%). In the CPH model, top risk factors for opioid-related hospitalization included alcohol dependence (hazards ratio [HR]: 2.45, 95% CI: 2.28 – 2.64), history of suicide attempts and self-harm (HR: 2.04, 95% CI:1.89 – 2.20) and history of substance abuse (HR: 1.27, 95% CI:1.14 – 1.43). Concomitant use of benzodiazepines and gabapentinoids were associated with 24% (HR: 1.24, 95% CI 1.21 – 1.26) and 18% (HR: 1.18, 95% CI 1.14 – 1.21) higher risks, respectively. Obesity and MME at initiation lacked statistical significance. Permutation importance highlighted antipsychotic and antidepressant use as top risk factors. The CPH and Random Survival Forest models achieved AUC values of 0.71 (95% CI: 0.70-0.72) and 0.68 (95% CI: 0.67-0.69), respectively.
Conclusion: The CPM based on CPH achieved better discrimination than the Random Survival Forest. Higher risks of opioid-related hospitalization were associated with concomitant use of benzodiazepines and gabapentinoids, prior alcohol dependence, and history of self-harm. Greater vigilance where these factors exist could guide targeted interventions to reduce opioid-related hospitalizations
To cite this abstract in AMA style:
Ramirez Medina C, Lunt M, Jenkins D, Dixon W, Peek N, Jani M. Development and Evaluation of Machine Learning Prediction Models for Hospitalizations Due to Opioid-Related Harms Among New Users with Rheumatic and Musculoskeletal Diseases [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/development-and-evaluation-of-machine-learning-prediction-models-for-hospitalizations-due-to-opioid-related-harms-among-new-users-with-rheumatic-and-musculoskeletal-diseases/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/development-and-evaluation-of-machine-learning-prediction-models-for-hospitalizations-due-to-opioid-related-harms-among-new-users-with-rheumatic-and-musculoskeletal-diseases/