Session Information
Date: Tuesday, November 9, 2021
Title: Abstracts: Spondyloarthritis Including PsA – Diagnosis, Manifestations, & Outcomes II (1919–1922)
Session Type: Abstract Session
Session Time: 2:00PM-2:15PM
Background/Purpose: Conventional radiography of the sacroiliac joints is still recommended as the first imaging method for the diagnosis of axial spondyloarthritis (axial SpA). In many clinical settings around the world, this is the only widely available imaging method to diagnose axial SpA. A high specificity of radiographic detection in the diagnostic setting is required to avoid improper diagnosis of axial SpA. We have recently developed a deep convolutional neural network (CNN) that was able to detect radiographic sacroiliitis with expert-like accuracy in two cohorts of patients with axial SpA, i.e., performing classification as radiographic or non-radiographic (Bressem KK, et al. Arthritis Res Ther 2021;23:106). The aim of the present study was to evaluate the performance of this CNN in detecting definite radiographic sacroiliitis in a diagnostic setting.
Methods: We evaluated sacroiliac radiographs of patients with chronic back pain who presented to a rheumatologist with a suspicion of axial SpA within the OptiRef study (Proft F, et al. Semin Arthritis Rheum 2020;50:1015-21). A total of 361 patients received a structured rheumatologic diagnostic work-up that resulted in the final diagnosis of axial SpA/no axial SpA. Radiographs of sacroiliac joints were evaluated according to the modified New York criteria; the consensus judgement of rheumatologist and radiologist on the presence of definite radiographic sacroiliitis ( >=grade 2 bilaterally or >=grade 3 unilaterally) was used as a reference. The predictions of the deep CNN’s inference on all available pelvic radiographs was compared to this reference judgement.
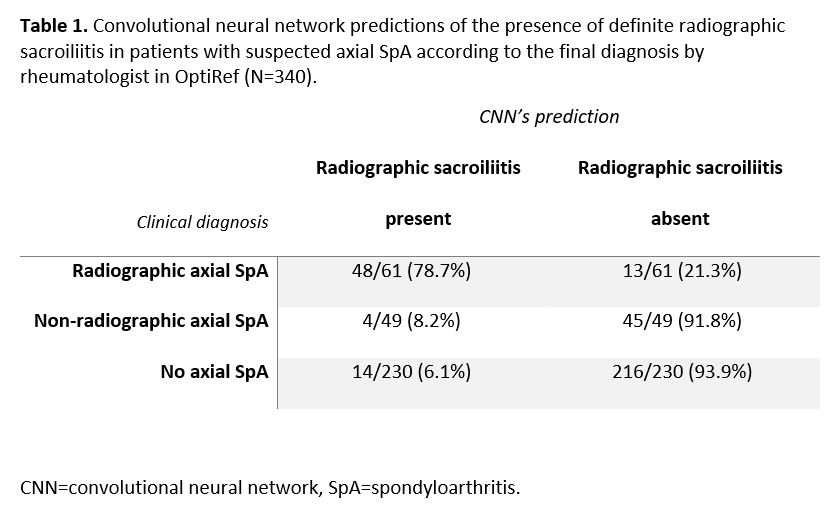
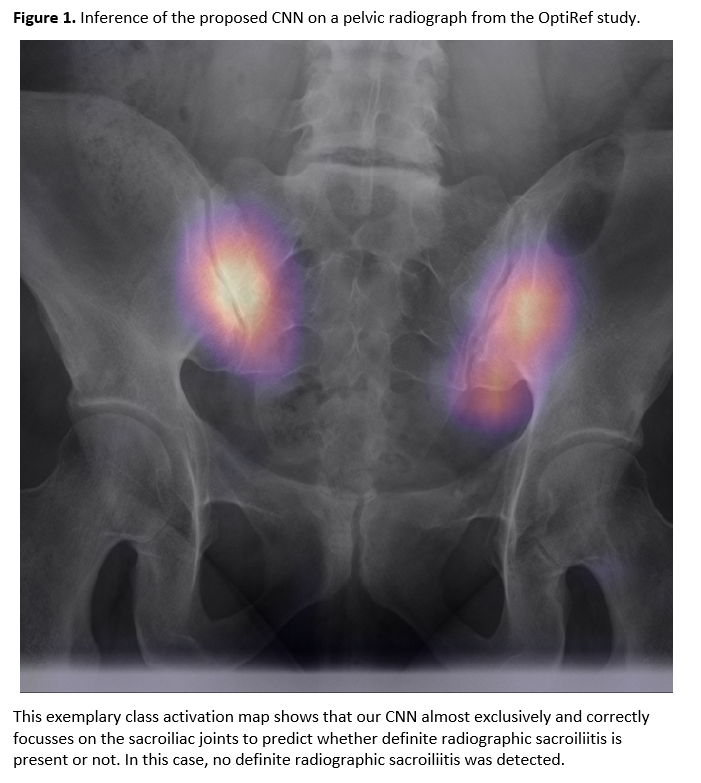
Results: Pelvic radiographs of 340 out of 361 patients (110 diagnosed with axial SpA including 61 patient with radiographic and 49 with non-radiographic axial SpA, and 230 without SpA) were available for the CNN evaluation. We used a balanced cutoff of 0.724 for the predictions of the model that was derived from the training and validation step previously. The deep CNN achieved a sensitivity of 79% for the diagnosis of radiographic axial SpA. The specificity of radiographic sacroiliitis detection was 94% (table 1). The area under the receiver operating characteristics curve for the prediction of the presence of definite radiographic sacroiliitis was 88%. The absolute agreement on the classification as radiographic or non-radiographic axial SpA between the CNN and the reference was 85%. Figure 1 shows an exemplary class activation map of our CNN.
Conclusion: The artificial neural network showed good generalizability and a high specificity with acceptable sensitivity in the detection of radiographic sacroiliitis when applied in the diagnostic setting of patients with chronic back pain and suspicion of axial SpA. Thus, the trained CNN can therefore be used by non-specialized centers as an assistant tool for interpretation of sacroiliac radiographs as a part of the diagnostic approach.
To cite this abstract in AMA style:
Poddubnyy D, Proft F, Hermann K, Spiller L, Niehues S, Adams L, Protopopov M, Rios Rodriguez V, Muche B, Rademacher J, Torgutalp M, Bressem K, Vahldiek J. Detection of Radiographic Sacroiliitis with an Artificial Neural Network in Patients with Suspicion of Axial Spondyloarthritis [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/detection-of-radiographic-sacroiliitis-with-an-artificial-neural-network-in-patients-with-suspicion-of-axial-spondyloarthritis/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/detection-of-radiographic-sacroiliitis-with-an-artificial-neural-network-in-patients-with-suspicion-of-axial-spondyloarthritis/