Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Rheumatologists are increasingly called upon to manage patients with inflammatory arthritis (IA) due to immune checkpoint inhibitor (ICI) therapy. The pathogenesis of ICI-IA is poorly understood, as are clinical risk factors for its development. Additionally, although clinical observations suggest that ICI treatment may affect symptoms of osteoarthritis (OA), whether OA is a risk factor for ICI-IA is unknown. We aimed to evaluate whether hip OA is associated with increased development of ICI-IA and whether either ICI-IA or OA affected mortality in a group of lung cancer patients treated with ICIs.
Methods: Patients were included if they were treated for lung cancer with anti-CTLA-4, anti-PD-1, and/or anti-PD-L1 therapies alone or in combination with chemotherapy and had a CT of the abdomen/pelvis (performed for cancer staging and monitoring) available within one month of starting ICI therapy. Patients were excluded if they had received less than 2 doses of ICI therapy or had bilateral hip replacement. Chart review determined presence of ICI-IA and other irAEs through 3/1/2024; patients had ICI-IA if it was documented in the medical record by a rheumatologist or oncologist or if there was documentation of new joint swelling after ICI start without another cause by a physician at an in person visit. End of follow up time was death or last contact in the electronic health record. Kellgren-Lawrence (KL) grading was applied to the hips on coronal slices of the CTs by a musculoskeletal radiologist. Those with KL grade of 2 or higher in either hip were classified as having hip OA. Overall survival was extracted from the Johns Hopkins Lung Cancer Precision Medicine Analytics Platform database. Incidence rates of ICI-IA were calculated per 1000 person years of follow up in patients with and without hip OA. Overall survival was compared by Kaplan-Meier curves and Cox proportional hazards.
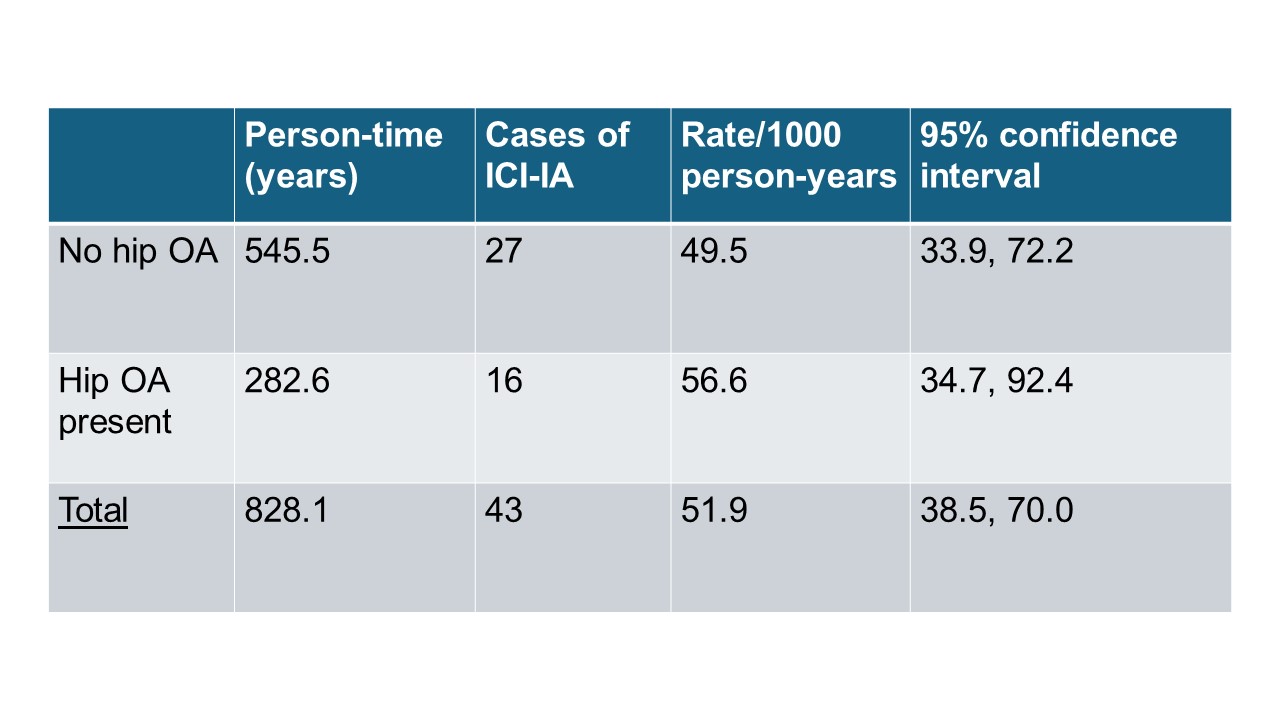
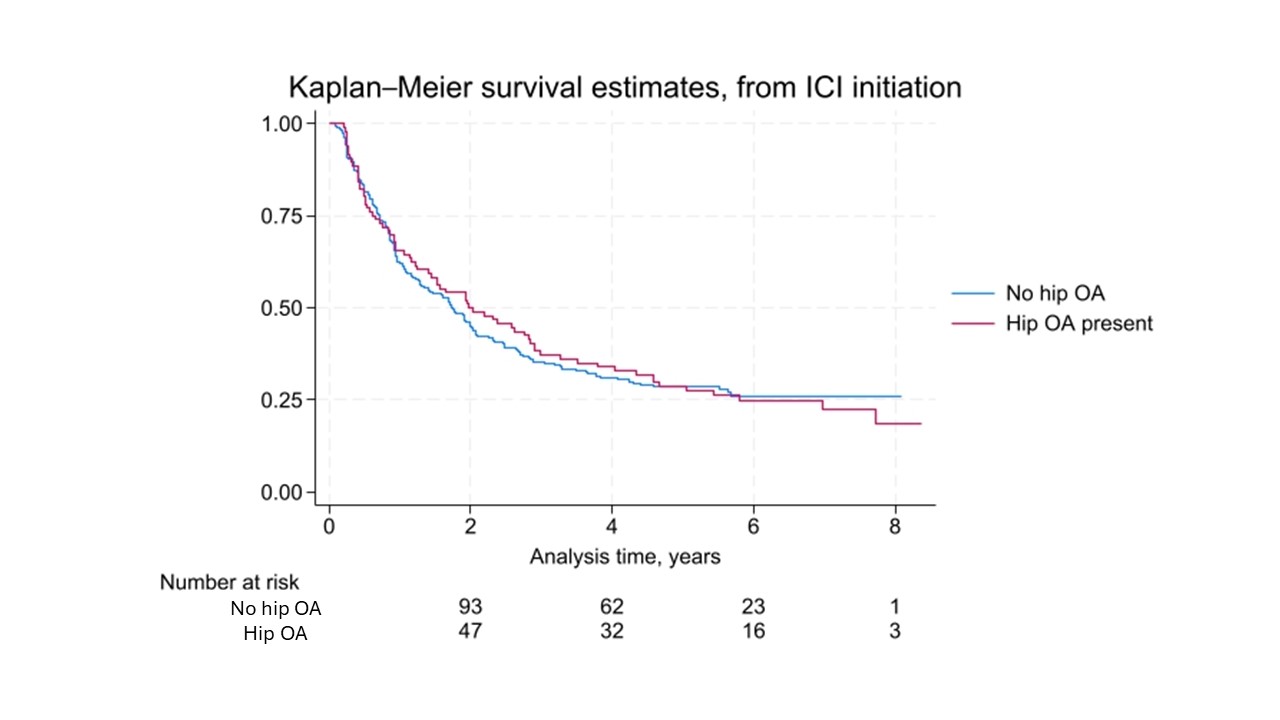
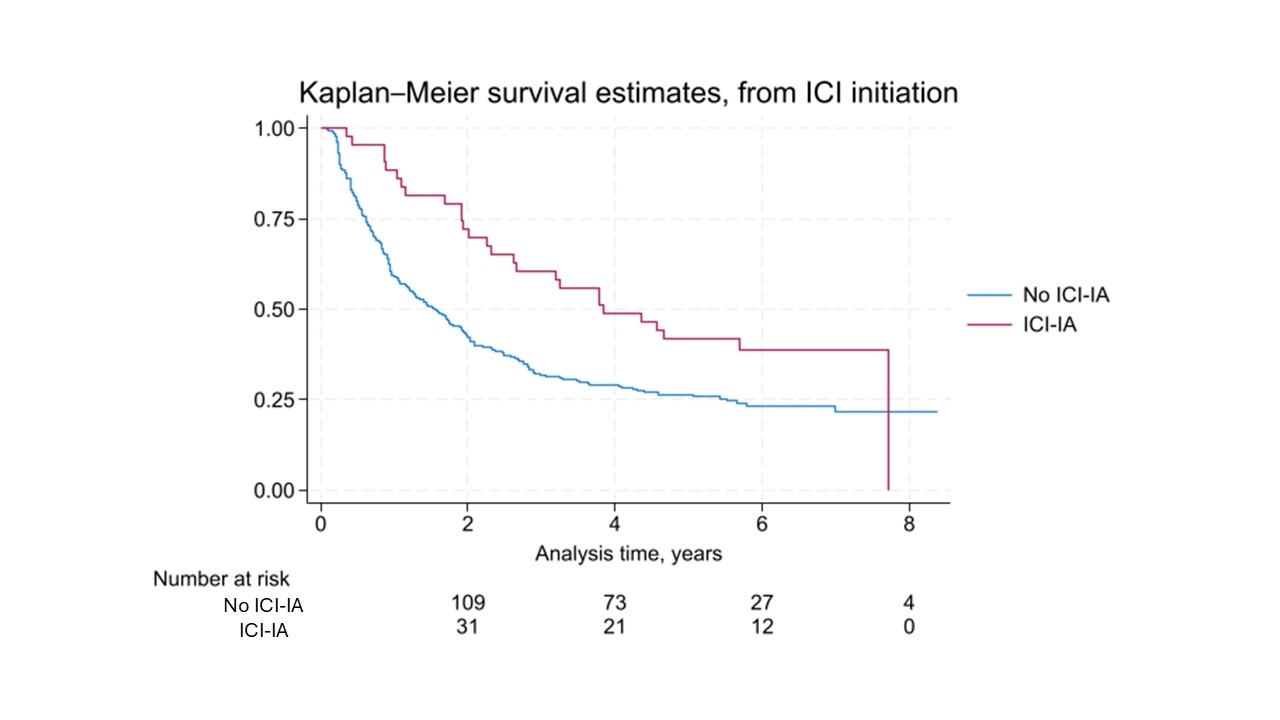
Results: A total of 302 patients were included with mean follow up of 2.7 years (SD 2.4). Average age was 65 (SD 10) and 45% were female. They received ICI therapy for an average of 246 days. 223 (73.8%) were deceased by the end of follow up. Overall, the cumulative incidence of ICI-IA was 51.9 cases/1000 person-years. Cumulative incidence of ICI-IA in those with hip OA was 56.6/1000 person-years, while in those without OA it was 49.5/1000 person-years, but the difference was not statistically significant (p=0.66). Survival did not differ by hip OA status (p=0.76, figure 1) but was improved in patients with ICI-IA (p = 0.0067, figure 2). There was a significantly decreased hazard of death in patients with ICI-IA in an unadjusted analysis (HR 0.57, p=0.006). When adjusting for age, sex, and ICI duration, a trend toward decreased death in those with ICI-IA persisted (HR 0.67, p=0.058). There was no significant change in mortality by presence of hip OA (HR 0.98, p =0.908)
Conclusion: Hip OA as determined from CT of the abdomen/pelvis was not significantly associated with development of ICI-IA in this cohort of lung cancer patients. ICI-IA was associated with decreased mortality and this trend persisted with adjustment for other factors. Further studies should evaluate risk factors beyond hip OA for ICI-IA development.
To cite this abstract in AMA style:
Cappelli L, Demehri S, Murray J, Brahmer J, Ghotbi E, Barasa D, Bingham C, Shah A. Cumulative Incidence of Immune Checkpoint Inhibitor-Induced Inflammatory Arthritis in Lung Cancer Patients with and Without Hip Osteoarthritis and Impacts on Survival [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/cumulative-incidence-of-immune-checkpoint-inhibitor-induced-inflammatory-arthritis-in-lung-cancer-patients-with-and-without-hip-osteoarthritis-and-impacts-on-survival/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/cumulative-incidence-of-immune-checkpoint-inhibitor-induced-inflammatory-arthritis-in-lung-cancer-patients-with-and-without-hip-osteoarthritis-and-impacts-on-survival/