Session Information
Date: Friday, November 6, 2020
Title: Epidemiology & Public Health Poster I: COVID-19 & Rheumatic Disease
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: The SARS CoV-2 pandemic has inspired new interest in understanding the fundamental pathology of pneumonia and Acute Respiratory Distress Syndrome (ARDS). SARS CoV-2 in humans is associated with a broad spectrum of clinical respiratory syndromes, ranging from mild upper airway symptoms to progressive life threatening pneumonia. A proportion of patients develop ARDS. Although evidence is emerging on risk factors, not much is known about the morphologic and molecular changes in the lungs of patients with Covid-19. Radiographically, peripheral ground glass opacities on CXR and CT scan fulfil the criteria for ARDS but are still not well characterized. What seems consistent is that ARDS and critical illness appear to develop most commonly between 1–2 weeks after the onset of symptoms. Some Covid-19 patients are at increased risk of developing respiratory failure which appears to be driven by hyper-inflammation, resembling cytokine storm syndrome (CSS). There are currently no approved pharmacological treatments; however several trials are on going at present. The lack of reliable clinical and serological predictors for deterioration is making it harder to triage and manage these patients appropriately. This study aimed at identifying potential predictors for outcomes, using baseline clinical parameters.
Methods: For this study, demographics, clinical and laboratory data, imaging and outcomes were collected for 592 patients with COVID 19 between February 20th and May 7th 2020 from a single centre in Essex, United Kingdom. 500 were included in final analysis. We used multivariable logistic regression models to identify risk factors.
Results: Refer to Tables 1&2. Mean age of the cohort was 69.4, 300(60%) were males. Majority were Caucasians, 436 (87%) and our cohort comprised of patients over 70, 290(58%). Most patients had 2 or more comorbidities 280(56%). Most common were hypertension 186(37 %), Cardiovascular disease 178(36 %) and Diabetes 128 (26 %). Cough was the common presentation 295(59%) followed by dyspnoea 294(58.8%) and fever 248(50 %.). Mean CRP was very high at baseline 111, neutrophil-lymphocyte ratio was 11.64 and baseline mean creatinine was 114. 44(8.8 %) had secondary bacterial infection.
The mean SpO 2/FIO 2 ratio (SFR) was 371 and 56 (11%) of patients fell into ARDS criteria and 181(36.7%) had acute lung injury. 66.4% had significant CXR findings including bilateral ground glass opacities and consolidation. 348(69.6%) required Oxygen, 56(11.2%) required CPAP and 64(12.8%) needed mechanical ventilation.
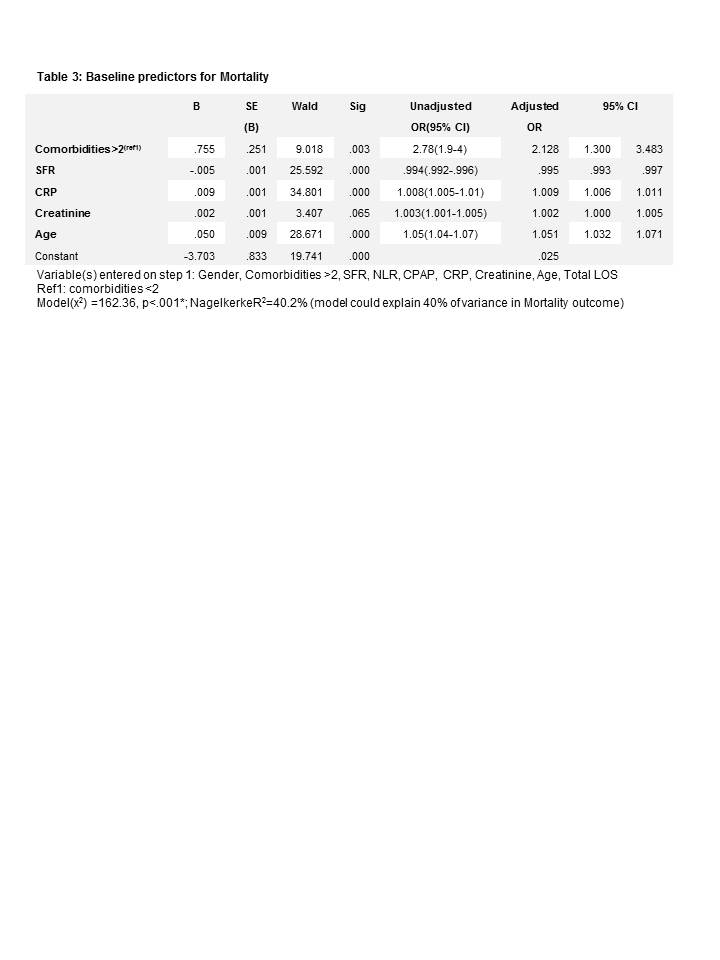
Of the 500, 193(38.6%) died and mean length of stay was 8.43 days. Baseline predictors for mortality were: comorbidities >2 OR 2.13(95% CI 1.30 – 3.48), CRP OR 1.01(95% CI 1.01 – 1.01), Creatinine OR 1.00 (95% CI 1.00 – 1.01), Age OR 1.05(95% CI 1.03 – 1.07). SFR had a trend towards increase mortality OR 0.99 (95% CI 0.99 – 0.10)
Conclusion: In this single centre study, older patients, comorbidities, baseline CRP and creatinine were risk factors for worse outcomes. Real-time consistent monitoring of SFR and inflammatory markers are essential in monitoring disease course, allowing for early intervention to improve patient outcomes.
To cite this abstract in AMA style:
Gokaraju S, Darda M, Warrier V, Duta I, Hayes F, Ahmed Y, Koduri G. COVID -19 Lung Inflammation – What Have We Learnt so Far ? [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/covid-19-lung-inflammation-what-have-we-learnt-so-far/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/covid-19-lung-inflammation-what-have-we-learnt-so-far/