Session Information
Session Type: Poster Session C
Session Time: 8:30AM-10:30AM
Background/Purpose: Class III obesity, defined by BMI >40kg/m2, is linked to increased risk of complications post total knee replacement (TKR). This has led to recommendations for weight loss before TKR and even institutional BMI cutoffs for TKR. Surgical and nonsurgical weight loss (NSWL) programs show variable efficacy, but the cost-effectiveness of alternative weight loss interventions prior to TKR has received little study.
Methods: We used the Osteoarthritis Policy Model, a validated widely published microsimulation of knee osteoarthritis (OA), to evaluate the cost-effectiveness of weight loss interventions for patients with advanced knee OA and class III obesity planning to undergo TKR. We considered five strategies: 1) no weight loss intervention, no TKR; 2) immediate TKR; 3) NSWL+TKR; 4) Laparoscopic Sleeve Gastrectomy (LSG)+TKR; 5) Roux-En-Y Gastric Bypass (RYGB)+TKR. In strategies 3-5, patients were evaluated for TKR one year after weight loss intervention start. We followed subjects in the model until death, recording quality-adjusted life years (QALYs) accrued, lifetime medical costs, and TKR utilization. We examined a cohort with WOMAC pain consistent with literature pre-TKR pain (WOMAC Pain (0-100): mean 54, SD 15). We used national databases and published data to estimate weight loss strategy efficacy (initial BMI lost: NSWL 0-20%; LSG 18-38%; RYGB: 23-47%), TKR efficacy (mean WOMAC Pain reduction: 16-38 points, stratified by pre-operative WOMAC pain), surgical costs (LSG $16,099; RYGB $18,042; TKR $18,642-$19,300, stratified by BMI), and costs and risks of complications and mortality attributable to LSG, RYGB, and TKR. In sensitivity analyses we varied: cost of health consequences of class II and III obesity, BMI cutoff and pain thresholds for TKR eligibility, LSG/RYGB pain efficacy, likelihood of complications from LSG/RYGB, and maximum years weight loss is maintained following LSG/RYGB. We discounted costs and QALYs at 3%/year and conducted analysis from a healthcare perspective. We calculated incremental cost-effectiveness ratios (ICERs) as the ratio of change in costs to change in QALYs for competing strategies in 2019 USD.
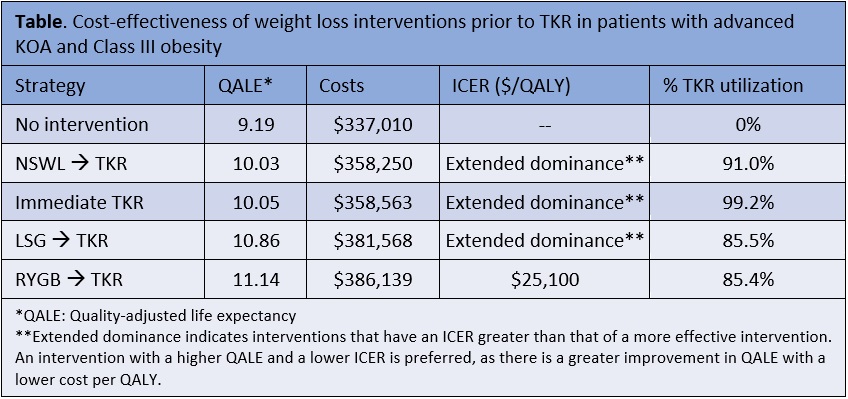
Results: Among patients with advanced knee OA and class III obesity, undergoing RYGB followed by TKR, if eligible, added 1.95 QALYs and $49,129 in medical costs in comparison to no interventions, resulting in an ICER of $25,100/QALY (Table). All other weight loss interventions were less economically efficient. Weight loss affected TKR usage; the percent of patients undergoing TKR ranged from 99.2% with immediate TKR (< 100% due to contraindications and mortality), 91.0% with NSWL, 85.5% with LSG, and 85.4% with RYGB (Table). ICERs were sensitive to the number of years weight loss was sustained, costs of obesity, LSG complication rates, and LSG/RYGB pain efficacy.
Conclusion: RYGB prior to TKR is a cost-effective strategy for addressing knee pain and obesity in patients with advanced knee OA and Class III obesity. TKR alone and NSWL or LSG prior to TKR are less economically efficient options compared to RYGB prior to TKR.
To cite this abstract in AMA style:
Kostic A, Leifer V, Neogi T, Hunter D, Suter L, Selzer F, Katz J, Losina E. Cost-effectiveness of Weight Loss Interventions Prior to Total Knee Replacement for Patients with Advanced Knee Osteoarthritis and Class III Obesity [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/cost-effectiveness-of-weight-loss-interventions-prior-to-total-knee-replacement-for-patients-with-advanced-knee-osteoarthritis-and-class-iii-obesity/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/cost-effectiveness-of-weight-loss-interventions-prior-to-total-knee-replacement-for-patients-with-advanced-knee-osteoarthritis-and-class-iii-obesity/