Session Information
Date: Monday, November 14, 2022
Title: Metabolic and Crystal Arthropathies – Basic and Clinical Science Poster
Session Type: Poster Session D
Session Time: 1:00PM-3:00PM
Background/Purpose: Gout is a highly prevalent inflammatory arthritis with increasing global disease burden in recent years.1,2 A recent analysis3 of the Multiethnic Cohort Study reported that, compared to White individuals, Native Hawaiian, Black, and Japanese-American individuals had 220%, 34%, and 14% higher risk of incident gout while Hispanic individuals had a 22% lower risk. Furthermore, once diagnosed with gout, data show minority patients may be less likely to receive appropriate gout care, such as urate-lowering therapy, in the ambulatory setting.4 How these disparities in background gout risk and suboptimal outpatient care translate into the risk of avoidable and costly health care utilization, such as emergency department (ED) visits and hospitalizations directly due to gout, remains largely unknown. Thus, we sought to examine the contemporary racial/ethnic disparities in ED visits and hospitalizations with a primary discharge diagnosis of gout in the US in 2019.
Methods: Using the latest available data (2019) from the National Emergency Department Sample (NEDS) and National Inpatient Sample (NIS), we compared the racial/ethnic differences in annual population rates of ED visits and hospitalizations for gout (primary discharge diagnosis) per capita (per 100,000 US adults using the 2019 age- and sex-specific US census data). We also examined the rates of ED visits and hospitalizations for gout per total US ED visits/hospitalizations, adjusting additionally for payer, region, and household income.
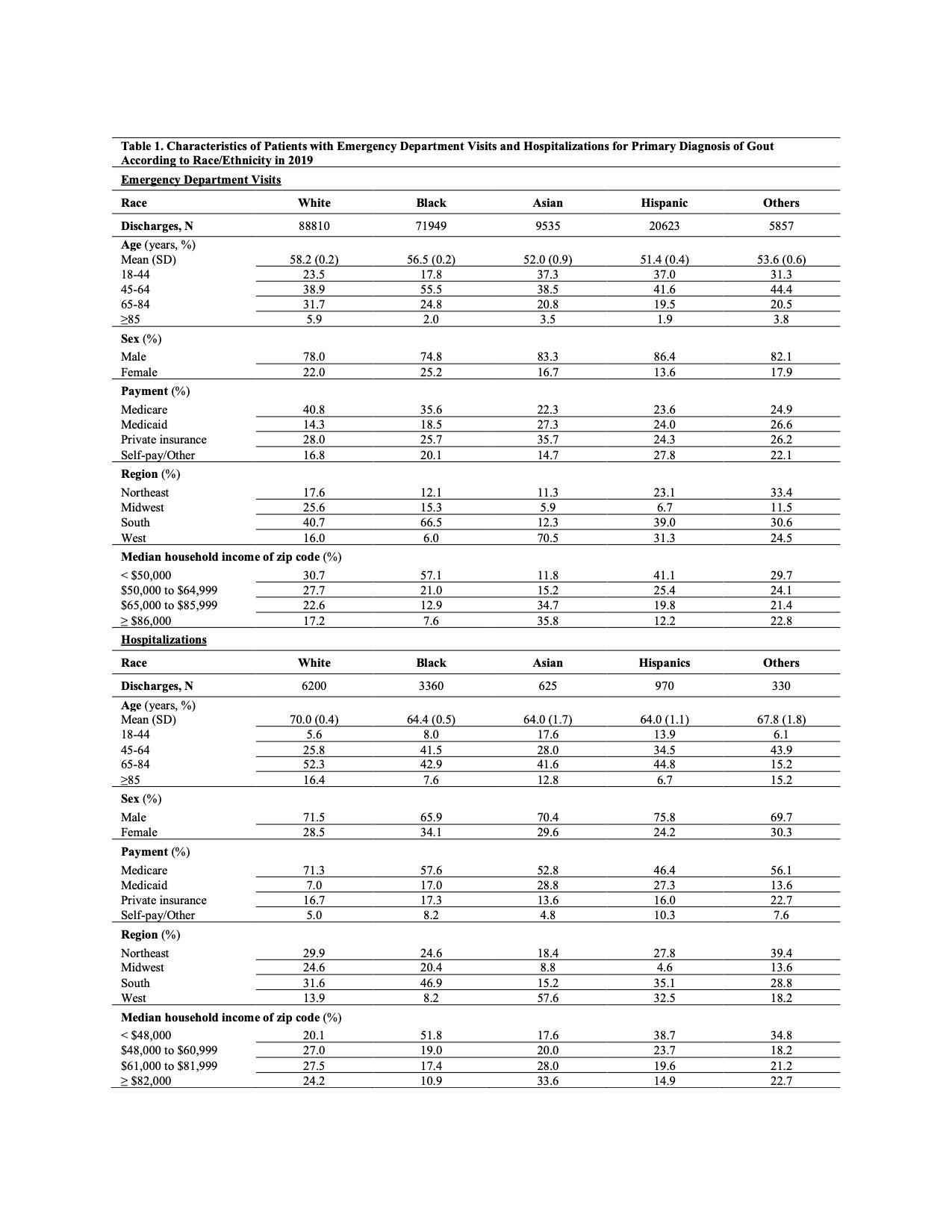
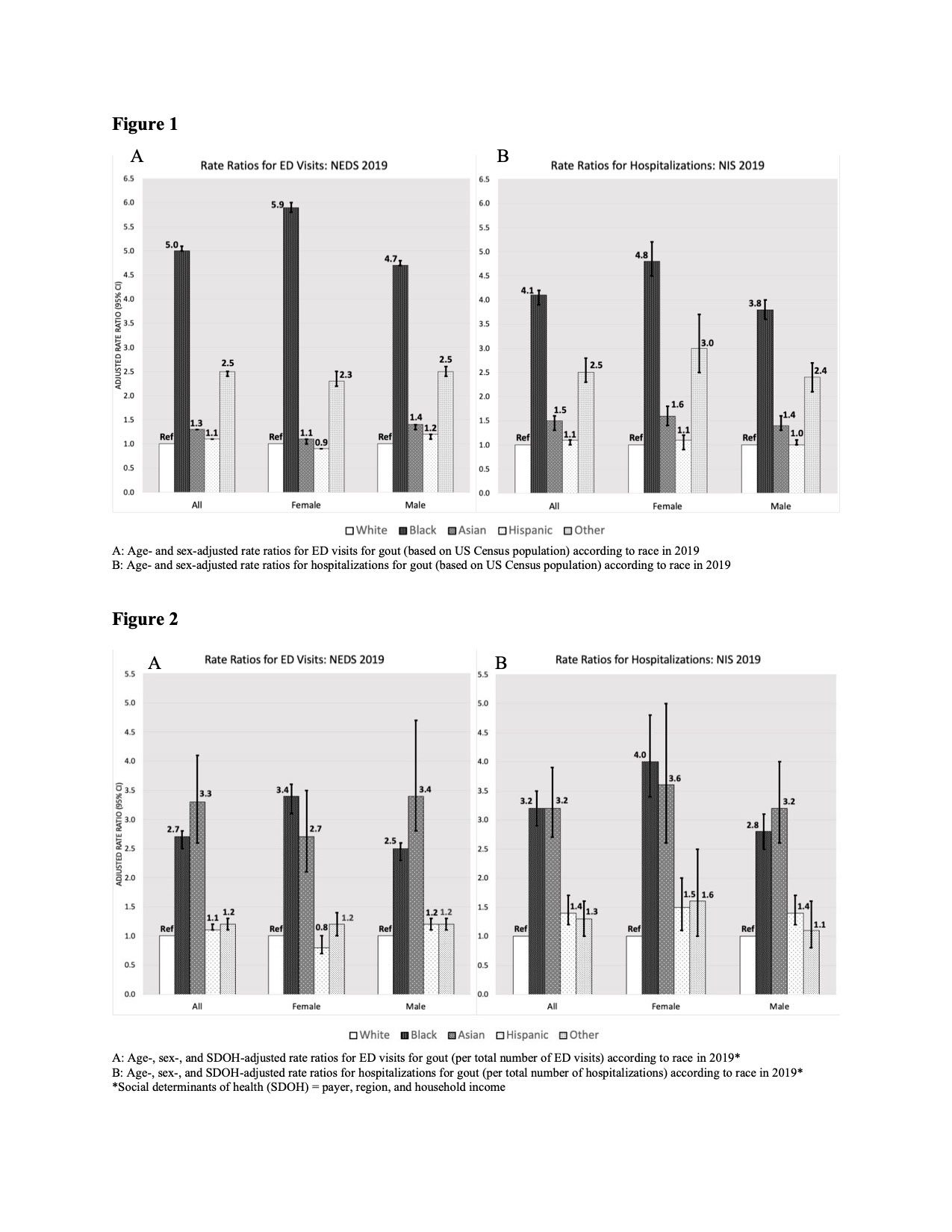
Results: We identified a total of 196,774 ED visits and 11,485 hospitalizations for a primary diagnosis of gout in the US in 2019 (Table 1). White individuals tended to be older than their racial/ethnic minority counterparts, particularly Asian and Hispanic individuals. The proportion of females tended to be higher among Black adults and lower among Hispanic adults (Table 1). The age- and sex-adjusted rate ratios per capita among US White, Black, Asian, and Hispanic patients for gout-primary ED visits were 1.0, 5.01 (95% CI, 4.96, 5.06), 1.29 (1.26, 1.31), 1.12 (1.10, 1.13) and for gout-primary hospitalizations were 1.0, 4.07 (3.90, 4.24), 1.46 (1.34, 1.58), and 1.06 (0.99, 1.13), respectively (Figure 1). The corresponding ratios per total US ED visits were 1.0, 3.17 (95% CI, 2.86, 3.50), 3.23 (2.71, 3.85), and 1.43 (1.21, 1.68); and per total hospitalizations were 1.0, 2.47 (2.32, 2.64), 3.43 (2.76, 4.72), and 1.21 (1.12, 1.31), respectively (Figure 2). These ratios were the largest among Black women both per capita and per total ED visits/hospitalizations.
Conclusion: These latest nationwide data indicate that gout-primary ED visits and hospitalizations are higher in all racial/ethnic minority patients than non-Hispanic White patients and are particularly high among Black patients. These findings implicate the role of suboptimal gout management for minorities, leading to avoidable healthcare utilization.
References:
1. Safiri et al., PMID 32755051
2. Xia et al., PMID 31624843
3. Thompson et al., PMID 35105711
4. Singh, J. PMID 23315156
To cite this abstract in AMA style:
Yokose C, mccormick n, lu n, johi a, Jackson L, Kohler M, Yinh J, zhang y, Hsu J, saag k, Choi H. Contemporary Racial/Ethnic Disparities in Emergency Department Visits and Hospitalizations for Gout in the United States – 2019 Nationwide Analysis [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/contemporary-racial-ethnic-disparities-in-emergency-department-visits-and-hospitalizations-for-gout-in-the-united-states-2019-nationwide-analysis/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/contemporary-racial-ethnic-disparities-in-emergency-department-visits-and-hospitalizations-for-gout-in-the-united-states-2019-nationwide-analysis/