Session Information
Date: Tuesday, October 28, 2025
Title: (2470–2503) Systemic Sclerosis & Related Disorders – Clinical Poster III
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Sjogren’s disease (SjD) is a common systemic autoimmune disorder characterized by progressive inflammation of the exocrine glands, resulting in dry eyes and dry mouth. Anti-Ro/SSA antibodies are the prototypical serologic marker of SjD, but they are also detected in other systemic autoimmune diseases, including systemic sclerosis (SSc). The prevalence and clinical implications of anti-Ro/SSA antibodies in SSc remain poorly understood. We hypothesized that anti-Ro/SSA antibodies confer distinct prognostic risk factors beyond sicca symptoms in patients with SSc. Our objective was threefold: 1) establish Ro/SSA seropositivity prevalence in SSc, 2) determine the frequency of sicca symptoms, and 3) assess if increased frequencies of specific organ complications were associated with Ro/SSA positivity.
Methods: We evaluated all new patients presenting with systemic sclerosis between 1980 and 2024 at a single university-dedicated scleroderma center. Participants underwent comprehensive serologic testing, including ANA, immunodiffusion, protein, and RNA immunoprecipitation (IP). Dedicated ELISA or IP screening for Ro/SSA antibodies was performed as clinically indicated. Demographics, clinical features, and survival were compared over long-term follow-up among patients who were anti-Ro/SSA positive, anti-Ro/SSA negative, or not tested.
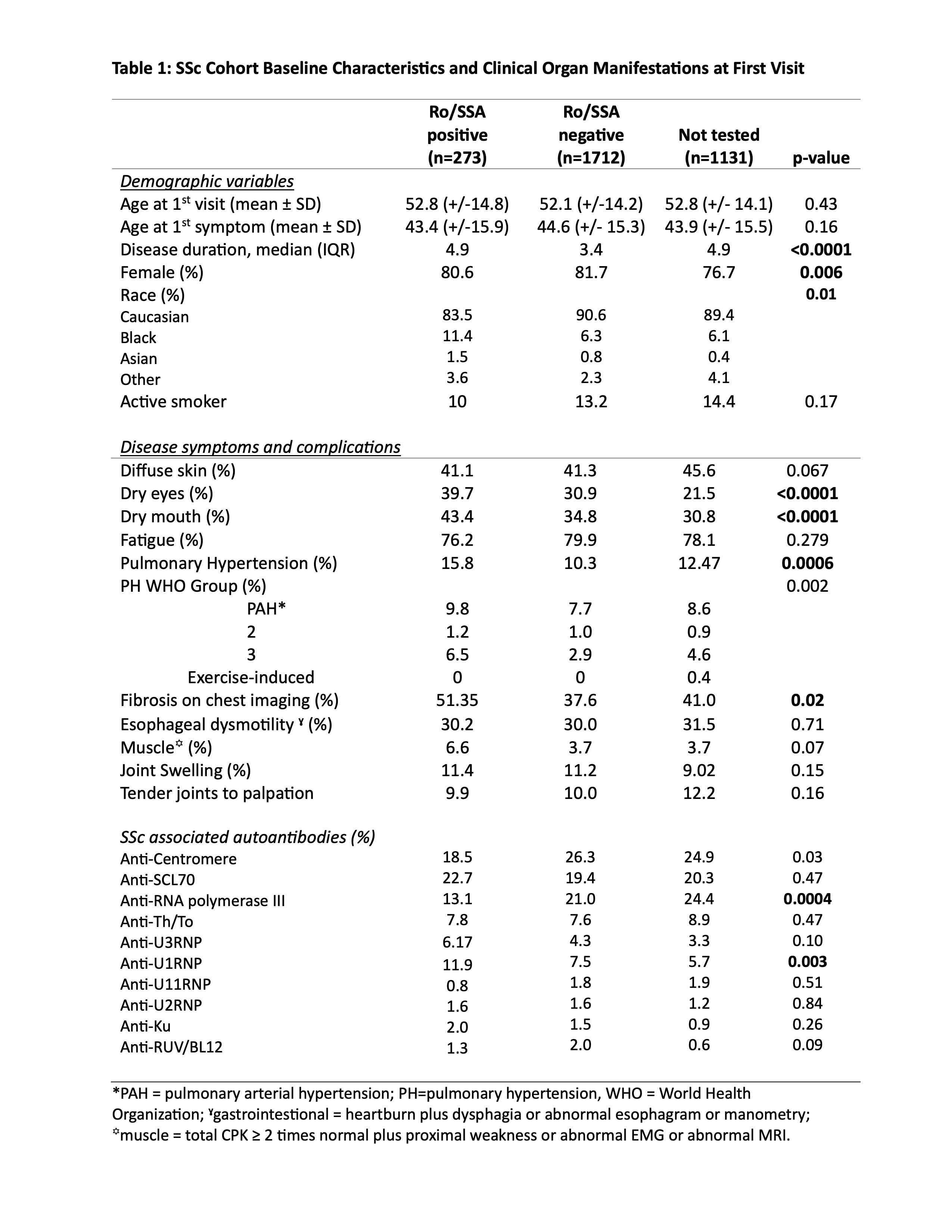
Results: There were 3,116 patients seen for an initial visit during this time period. In the cohort, 1,985 underwent anti-Ro/SSA testing. Amongst those tested, 13.8% (273/1,985) were anti-Ro/SSA positive. Amongst the concomitant SSc antibodies, SSA/Ro positivity occurred significantly more frequently with anti-U1RNP positivity, and significantly less with anti-RNA polymerase III antibodies (Table 1), even after correcting for multiple comparisons amongst the antibodies.Despite the presence of anti-Ro/SSA antibodies, only 47% of patients had objective dry eyes and 45% reported dry mouth, suggesting these antibodies may occur in the absence of a full SjD phenotype.SSA positivity was not associated with a difference in cutaneous subtype. It was, however, associated with significantly higher rates of pulmonary fibrosis by imaging Table 1& 2). Not surprisingly, the lowest mean FVC was lower in Ro/SSA positive patients. Interestingly, there were higher rates of pHTN (Table 1 & 2). Kaplan-Meier survival analyses showed reduced 5- and 10-year survival among anti-Ro/SSA positive and untested patients compared to anti-Ro/SSA negative individuals (Figure 1).
Conclusion: Here, we show that 14% of SSc tested patients had Ro/SSA antibodies. As expected, anti-Ro/SSA patients were more likely to have sicca symptoms. Notably, anti-Ro/SSA positive patients had significantly increased rates of pulmonary fibrosis and pHTN. Anti-Ro/SSA positive patients also demonstrated reduced survival at 5 and 10 years. Untested individuals showed a similar survival decrement. Taken together, these data show that anti-Ro/SSA positivity identifies a clinically meaningful SSc phenotype with increased pulmonary involvement and worse prognosis, highlighting its potential role in clinical care and future research.
To cite this abstract in AMA style:
Gordon R, Wunsch L, Lauffoon M, Medsger, Jr T, Domsic R. Concomitant Anti-Ro/SSA Antibodies in Systemic Sclerosis Patients is Associated with Risks Beyond Dryness [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/concomitant-anti-ro-ssa-antibodies-in-systemic-sclerosis-patients-is-associated-with-risks-beyond-dryness/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/concomitant-anti-ro-ssa-antibodies-in-systemic-sclerosis-patients-is-associated-with-risks-beyond-dryness/

.jpg)
.jpg)