Session Information
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Tubulointerstitial injury is a strong predictor of progression to kidney failure in lupus nephritis (LN). Prior animal studies suggest intrarenal complement activation has an important and underrecognized role in tubulointerstitial fibrosis in LN, yet this has not been shown in LN patients. This study aimed to identify complement markers of tubulointerstitial fibrosis in LN and potential therapeutic targets. Tubular complement gene expression in LN kidneys from patients with and without interstitial fibrosis/tubular atrophy (IFTA) was compared using scRNA-seq data.
Methods: We used data from the Accelerating Medicine Partnership/ Multi-Ethnic Translational Research Optimization Lupus cohort, which applied scRNA-seq to 20 LN kidney tissue samples [1]. Cells between 200 and 2500 detected features were included. The data was normalized, scaled, and underwent principal component analysis and clustering using Uniform Manifold Approximation and Projection plots to identify distinct cell subtypes. Specific marker genes were used to identify the kidney tubular cell subtypes: ALDOB (proximal tubules), UMOD (loop of Henle), CALB1 (distal convoluted tubules), and SLC4A1/TMEM213 (collecting duct). Complement gene expression was compared between LN patients with and without IFTA in the overall tubular cells and in each tubular cell subtypes using two approaches: 1) subject-based analysis where the average gene expression per subject was calculated and compared between the groups using the Wilcoxon rank sum test. 2) single-cell analysis using a linear mixed effects model. IFTA was defined as ≥10% of interstitium with fibrosis and atrophy.
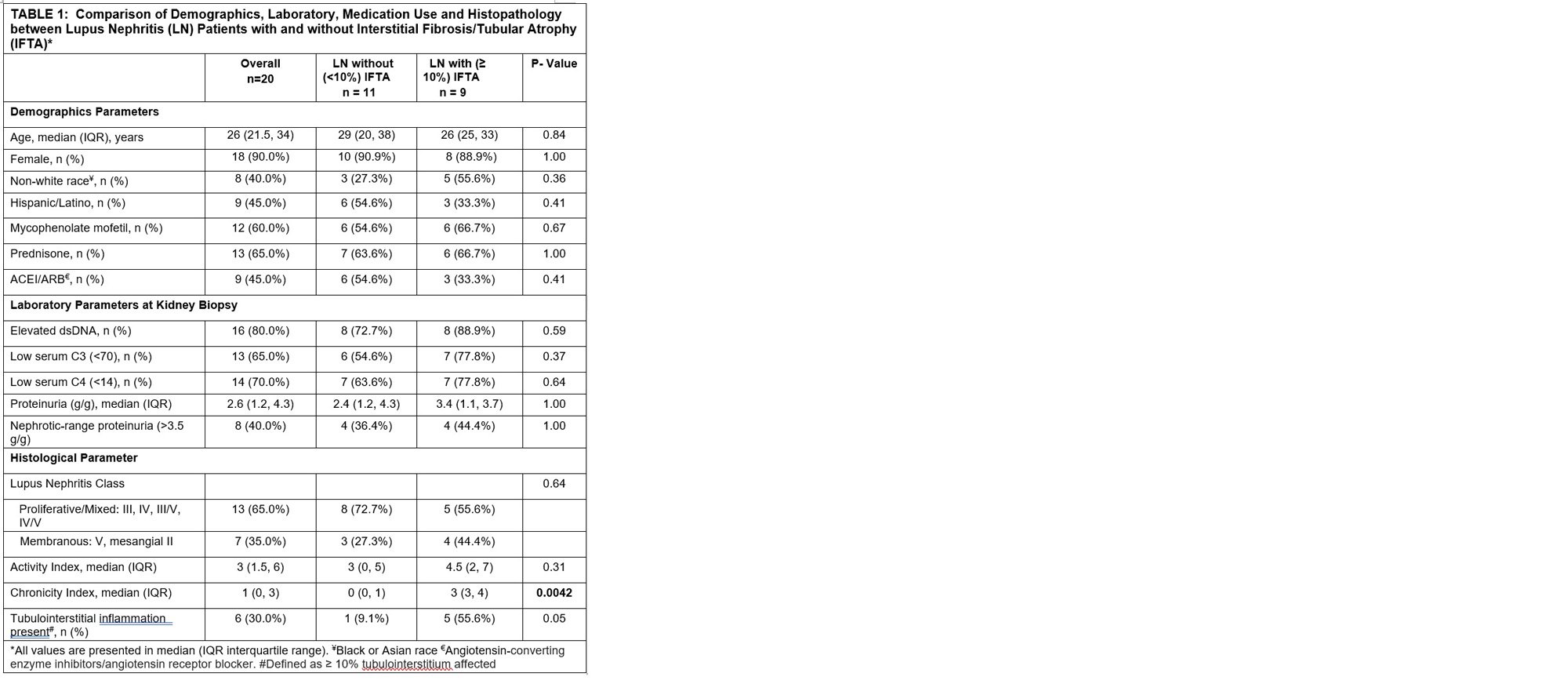
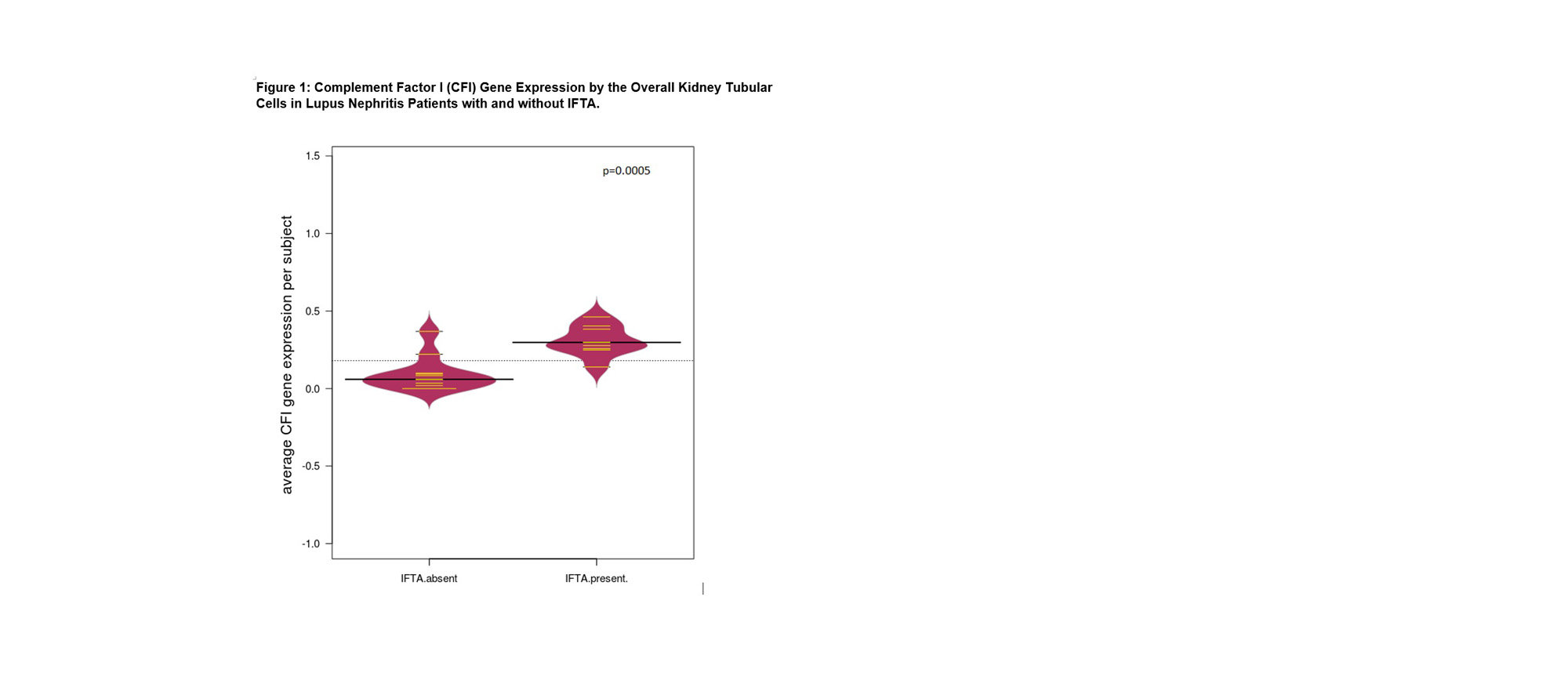
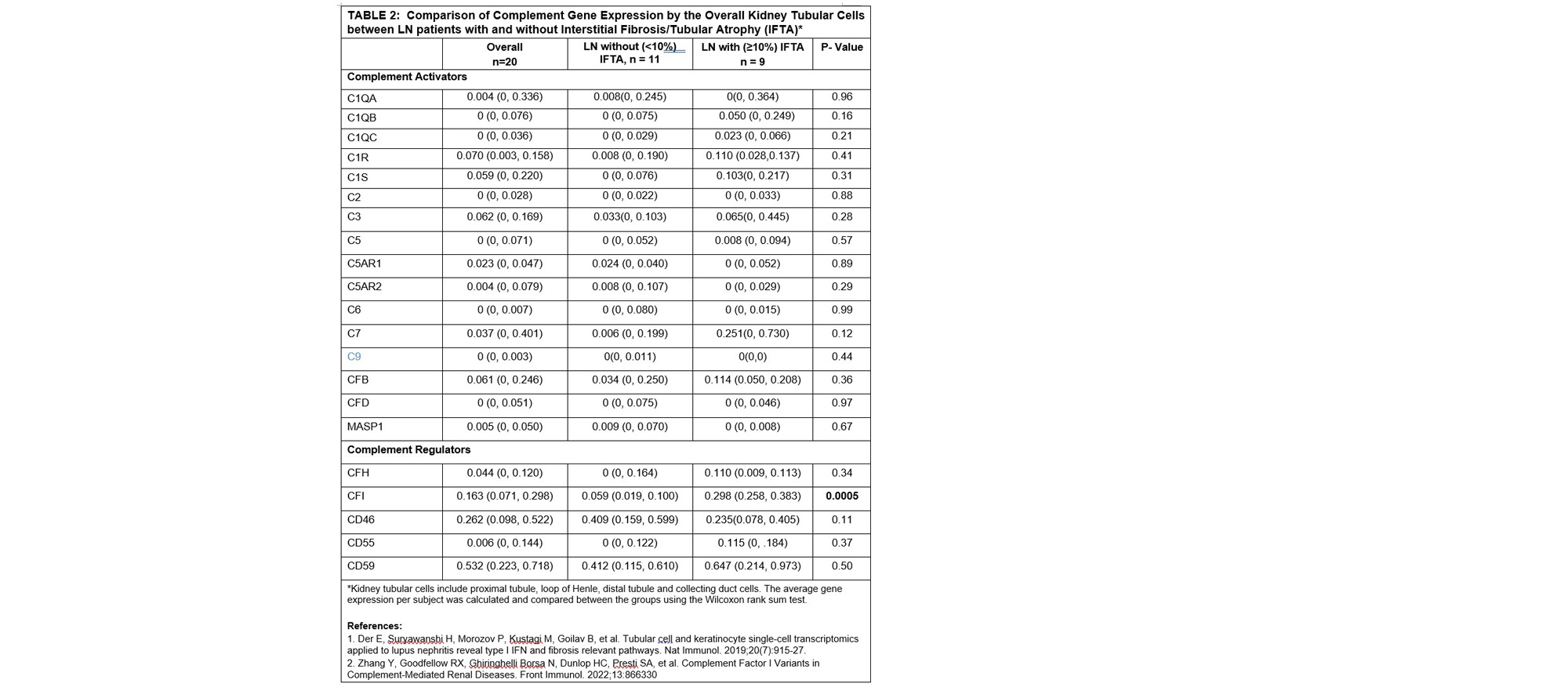
Results: Of the 20 LN patients, 9 had IFTA on kidney biopsy. Table 1 compares demographics, medication use, laboratory, and histopathology between LN patients with (≥ 10%) and without (< 10%) IFTA on biopsy. LN patients with IFTA had a higher proportion with tubulointerstitial inflammation as compared with those without IFTA (56% vs. 1%, p=0.05) and higher chronicity index median score 3 (IQR= 3, 4) vs 1(0,1). There was no difference in other variables. A total of 1162 kidney tubular cells were identified: 287 proximal tubular, 171 loop of Henle, 587 distal tubular and 117 collecting duct cells. LN patients with IFTA had significantly higher overall tubular expression of Complement Factor I (CFI) as compared to those without IFTA: median average expression 0.298 (0.258, 0.383) vs. 0.059 (0.019, 0.100), p=0.0005, Figure 1. No differential expression of other complement genes was found (Table 2). When evaluating each tubular cell subtype, no difference in average CFI expression was found. Single cell analysis also showed increased overall tubular expression of CFI (β=0.27, SE=0.05, p< 0.001) and C7 (β=0.31, SE=0.15, p=0.049) among LN patients with IFTA. Specifically, CFI expression was increased in the distal tubular cells (β=0.27, SE=0.06, p< 0.001) but not in the other tubular cell subtypes.
Conclusion: This study identifies CFI, a regulator of the alternative complement pathway, as a potential marker of IFTA in LN. Increased CFI has been found in other kidney diseases [2] and may overcompensate for a dysfunctional complement system.
To cite this abstract in AMA style:
Wang S, Greally J, Suzuki M, Moon J, Wang T, Saenger Y, Rovin B, Kahlenberg J. Complement Factor I (CFI) Gene Expression by Kidney Tubular Cells Is Increased in Lupus Nephritis Patients with Interstitial Fibrosis and Tubular Atrophy [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/complement-factor-i-cfi-gene-expression-by-kidney-tubular-cells-is-increased-in-lupus-nephritis-patients-with-interstitial-fibrosis-and-tubular-atrophy/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/complement-factor-i-cfi-gene-expression-by-kidney-tubular-cells-is-increased-in-lupus-nephritis-patients-with-interstitial-fibrosis-and-tubular-atrophy/