Session Information
Date: Sunday, October 26, 2025
Title: (0430–0469) Rheumatoid Arthritis – Diagnosis, Manifestations, and Outcomes Poster I
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Rheumatoid arthritis (RA) is a chronic autoimmune disease that manifests as either seropositive or seronegative subtypes. Seropositive RA, characterized by the presence of autoantibodies such as RF and ACPA, is often linked to more severe joint damage and systemic complications. In contrast, seronegative RA has a less defined clinical profile but may still present with significant comorbidities. This study aims to compare clinical outcomes between these RA subtypes using real-world data from the TriNetX Research Network.
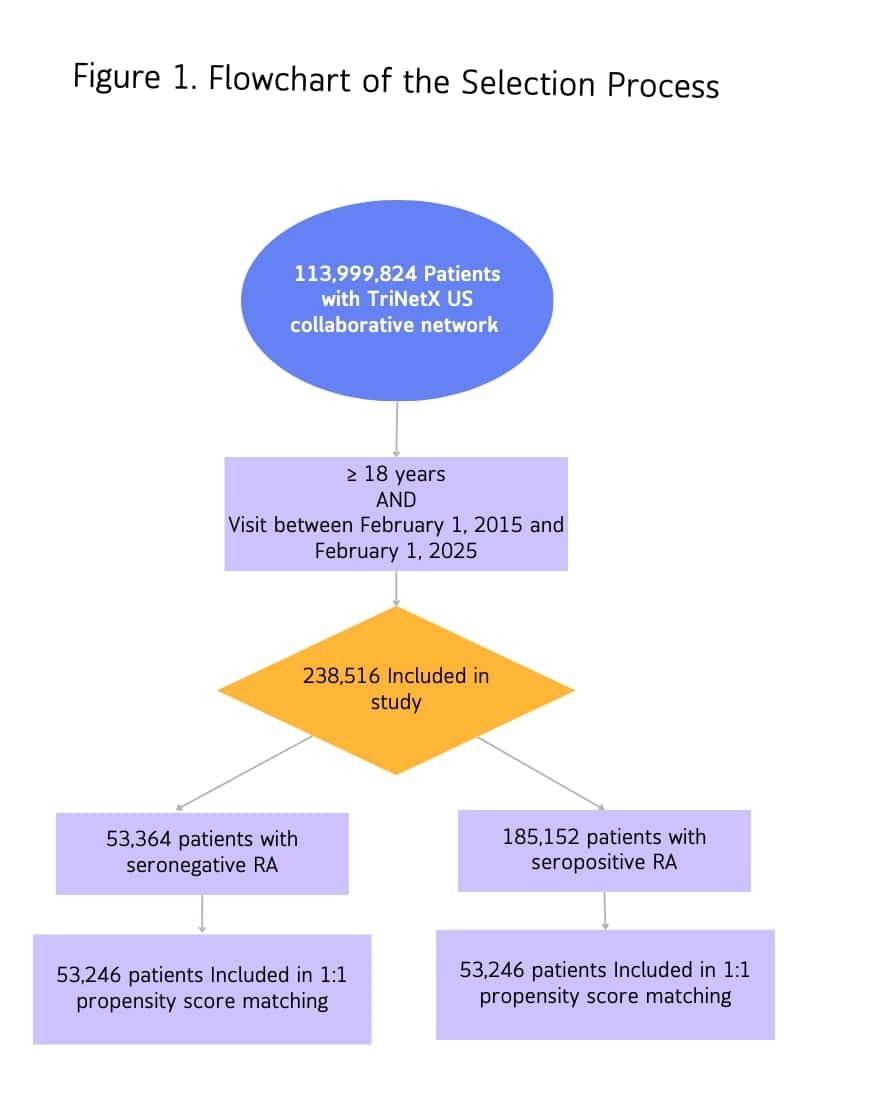
Methods: A retrospective cohort study was conducted to analyze adult patients diagnosed with rheumatoid arthritis (RA) between 2015 and 2025. Patients were categorized as either seropositive or seronegative based on the International Classification of Diseases, 10th Revision (ICD-10) codes. To reduce confounding and ensure comparability between groups, propensity score matching (PSM) was applied to balance key baseline characteristics, such as age, sex, comorbidities, and other rheumatologic diseases. Following matching, outcomes were compared between the two groups over a follow-up period of 10 years. Figure 1 illustrates the selection process. The primary outcome was all-cause mortality. Other outcomes included steroid dependence, disease-modifying antirheumatic drug (DMARD) use, RA-related joint damage, interstitial lung disease (ILD), and coronary artery disease (CAD).
Results: Among 106,492 matched patients (53,246 per cohort), seropositive RA patients had significantly higher all-cause mortality (OR: 1.24; p < 0.001). Kaplan-Meier analysis demonstrated lower survival probabilities in the seropositive group (76.51% vs. 81.68%; log-rank p < 0.001), with a hazard ratio of 1.21 (95% CI: 1.16–1.27), indicating a significantly increased risk. The use of DMARDs was more frequent in seropositive patients (OR: 1.35; p < 0.001), and steroid dependence was more common (OR: 1.18; p < 0.001). Additionally, seropositive patients had a higher risk of RA-related joint damage (OR: 1.24; p < 0.001). Furthermore, the incidence of ILD (OR: 2.42; p < 0.001), chronic CAD (OR: 1.11; p < 0.001), as well as acute coronary syndrome (ACS) (OR: 1.10; p = 0.008) were significantly higher (Table1) (Figure 2).
Conclusion: This study highlights significant differences in clinical outcomes between seropositive and seronegative RA patients. Seropositive RA was associated with higher all-cause mortality, greater steroid dependence, and more frequent use of DMARDs. Additionally, seropositive patients had a higher risk of RA-related joint damage, interstitial lung disease, and coronary artery disease. These findings highlight the more aggressive nature of seropositive disease and its extra-articular involvement, emphasizing the need for early and targeted interventions in this subgroup and reinforce the importance of autoantibody status in prognostication and risk stratification for RA patients.
.jpg) Comparative Outcomes in Seropositive and Seronegative Rheumatoid Arthritis
Comparative Outcomes in Seropositive and Seronegative Rheumatoid Arthritis
To cite this abstract in AMA style:
Alomari A, Elmusa R, Shah N, Rodriguez M, Alawneh D. Comparative Outcomes in Seropositive and Seronegative Rheumatoid Arthritis: A Retrospective Cohort Study [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/comparative-outcomes-in-seropositive-and-seronegative-rheumatoid-arthritis-a-retrospective-cohort-study/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/comparative-outcomes-in-seropositive-and-seronegative-rheumatoid-arthritis-a-retrospective-cohort-study/

.jpg)