Session Information
Date: Tuesday, November 7, 2017
Title: Osteoarthritis – Clinical Aspects Poster II: Observational and Epidemiological Studies
Session Type: ACR Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Inflammation contributes to OA disease pathogenesis. Subsets of knee OA patients with peripheral blood leukocyte (PBL) detected inflammatory gene expression profiles exhibit more rapid radiographic joint space narrowing (JSN). Bone marrow lesions (BMLs) on baseline knee MRI also predict JSN. We investigated whether the combination of the PBL inflammatory transcriptome(s) together with medial BML enhanced the ability of either alone to predict radiographic knee OA progression.
Methods: PBL inflammatory gene expression (IL-1, TNFα, COX-2) and 3T knee MRI were assessed in 111 patients with symptomatic medial knee OA and BMI<33. At baseline and 24 months, subjects underwent standardized fixed-flexion knee radiographs, scored for joint space width (JSW) by a musculoskeletal radiologist blinded to subject data; a separate, also blinded radiologist scored MRIs for BMLs using the whole-organ MRI scoring method scoring system. JSN was determined as medial JSW change over the study period. Radiographic progressors were defined by various cut-points of JSN (JSN>0.0mm, >0.2mm, and >0.5mm) and were compared to nonprogressors (JSN ≤0.0 mm). Logistic regression model was fit with 10-fold cross validation and repeated 100 times. Models were evaluated by area under the receiver operating characteristic curve (AUC) on test data. P values were obtained from DeLong test comparing models’ AUC to 0.5.
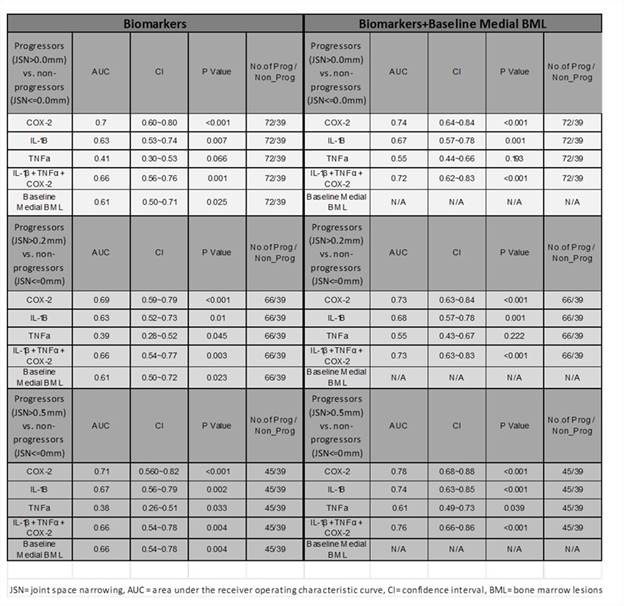
Results: Progressors by any JSN cut-point had significantly higher baseline medial BML scores (1.42±2.11, 1.45±2.13 and 1.78±2.23 for JSN>0.0mm, >0.2mm, and >0.5mm, respectively; p=0.025, 0.021, and 0.003) than nonprogressors (0.59±1.14). Baseline medial BML scores distinguished progressors by any level of JSN, from non-progressors in multivariate analyses (Table1; AUC 0.61, p=0.025; AUC 0.61, p=0.023, AUC 0.66, p=0.004, for JSN>0.0mm, >0.2mm, and >0.5mm, respectively). Elevated baseline PBL inflammatory gene expression also predicted JSN at all levels of progression, with COX-2 being the strongest predictor (Table 1). The combination of baseline medial BML scores with PBL inflammatory transcriptome markers, especially that of BML and PBL COX-2 expression (AUC 0.78, p<0.001 for JSN >0.5mm), yielded improved predictive power than any of the individual biomarkers alone (Table 1).
Conclusion: The combination of PBL-based inflammatory transcriptome and MRI-based medial BML biomarkers improves the prognostic utility to predict knee OA radiographic progression.
To cite this abstract in AMA style:
Krasnokutsky Samuels S, Zhou H, Attur M, Samuels J, Chang G, Bencardino J, Ma S, Rybak L, Abramson SB. Combinatorial Peripheral Blood Inflammatory and MRI-Based Biomarkers Predict Radiographic Joint Space Narrowing in Knee OA [abstract]. Arthritis Rheumatol. 2017; 69 (suppl 10). https://acrabstracts.org/abstract/combinatorial-peripheral-blood-inflammatory-and-mri-based-biomarkers-predict-radiographic-joint-space-narrowing-in-knee-oa/. Accessed .« Back to 2017 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/combinatorial-peripheral-blood-inflammatory-and-mri-based-biomarkers-predict-radiographic-joint-space-narrowing-in-knee-oa/