Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Chronic autoimmune and inflammatory diseases are associated with an increased prevalence of various comorbidities, which may impact both prognosis and therapeutic strategies. EULAR recommends systematic identification, prevention and screening of key comorbid conditions in this population.
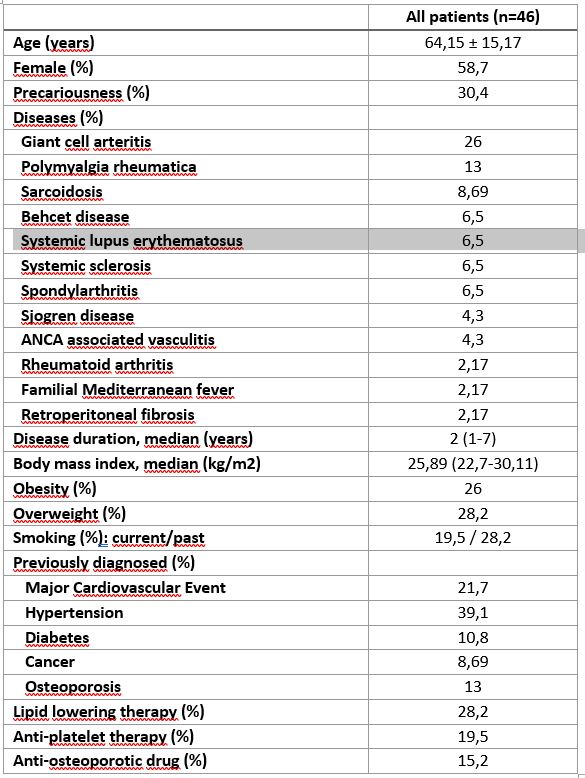
Methods: Since January 1st, 2025, the PREDIRE cohort has included consecutive adult patients with chronic autoimmune or inflammatory diseases undergoing a multimorbidity assessment during a one-day hospitalization. Collected data include sociodemographic and anthropometric characteristics, medical history, current treatments, cardiovascular risk factors, osteoporosis risk, and infectious risk evaluation (including dental follow-up and vaccination status). At the end of the assessment, individualized recommendations are issued for both the patient and their primary care physician.
Results: A total of 46 patients were included, with a mean age of 64.2 (±15.2) years . Autoimmune or inflammatory diseases were giant cell arteritis (26%), polymyalgia rheumatica (13%), sarcoidosis (8.7%), Behçet’s disease, systemic lupus erythematosus, systemic sclerosis , spondyloarthritis (6.5%), Sjogren disease (4.3%), ANCA-associated vasculitis (4.3%), or rheumatoid arthritis, familial mediterranean fever, or retroperitoneal fibrosis (2.17% each). The median duration of the disease was 2 years (IQR: 1–7).Regarding cardiovascular comorbidities, 21.7% had a history of major cardiovascular event, 38.1% had hypertension and 10.9% had diabetes.Obesity was observed in 26% of patients, while 28.2% were overweight. Physical inactivity was reported in 34.7% of patients. Active smoking was reported in 19.5% of cases and 28.2% had a history of smoking.Cardiovascular risk, estimated using the SCORE2 algorithm, showed that 65.2% of patients were at high or very high risk. Target LDL cholesterol levels were achieved in only 19.5% of patients.A risk of sleep apnea was identified in 21.2% of patients.While osteoporosis was previously known in 13% of patients, the assessment revealed newly diagnosed osteopenia in 34% and osteoporosis in 15.2%. Vitamin D deficiency was identified in 65% of patients, and inadequate calcium intake was noted in 71.7% of cases. Despite being indicated, osteoporosis treatment was lacking in 26% of patients.Dental follow-up was indicated in 21.7% of patients. Vaccination schedules needed updating in 84.7% of patients.In 54.3% of cases, cancer screening was outdated or incomplete, warranting an update of the recommended evaluations
Conclusion: The first data from the PREDIRE cohort highlight the high burden of comorbidities among patients with chronic autoimmune and inflammatory diseases. The implementation of a standardized, one-day multimorbidity screening approach allowed for the early identification of unrecognized or under-managed comorbid conditions, particularly in cardiovascular, bone, infectious, and cancer-related domains. These findings support the clinical utility of systematic comorbidity screening in improving patient care and guiding personalized preventive strategies.
To cite this abstract in AMA style:
Michaud M, Arlet C, Bournazeau J, de Maupeou F, Gaston J, Mermet S, Coulier H, Oustalet M, Raspaud C, Maurice C, Recipon S, Verplancken C, Paricaud K, Astudillo L. Clinical Relevance of Systematic Comorbidity Screening in Autoimmune and Inflammatory Diseases [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/clinical-relevance-of-systematic-comorbidity-screening-in-autoimmune-and-inflammatory-diseases/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/clinical-relevance-of-systematic-comorbidity-screening-in-autoimmune-and-inflammatory-diseases/

.jpg)