Session Information
Session Type: Poster Session D
Session Time: 1:00PM-3:00PM
Background/Purpose: Sarcoidosis is a multiorgan granulomatous disease with a prevalence of 60 per 100,000 in the United States.1 Given the low prevalence of both sarcoidosis and connective tissue disease (CTD) such as rheumatoid arthritis (RA) and systemic lupus erythematosus (SLE), it is rare to find both in the same patient, though several case reports suggest an association between the two2. In this study, we evaluate patients who have sarcoidosis and CTD and aim to describe clinical features associated with the development of both diagnoses.
Methods: This was a retrospective chart review performed between January 1, 2007 and December 31, 2019. Adult patients identified via ICD codes were included if they carried a diagnosis of sarcoidosis with CTDs, including RA, SLE, scleroderma, Sjogren syndrome, polymyalgia rheumatica, or spondyloarthropathy. Patients with sarcoidosis had a tissue biopsy showing noncaseating granulomas or were identified clinically by a rheumatologist or pulmonologist. Patients with CTD were diagnosed by a rheumatologist. Data on time of diagnosis, demographics, clinical characteristics, and therapy were evaluated.
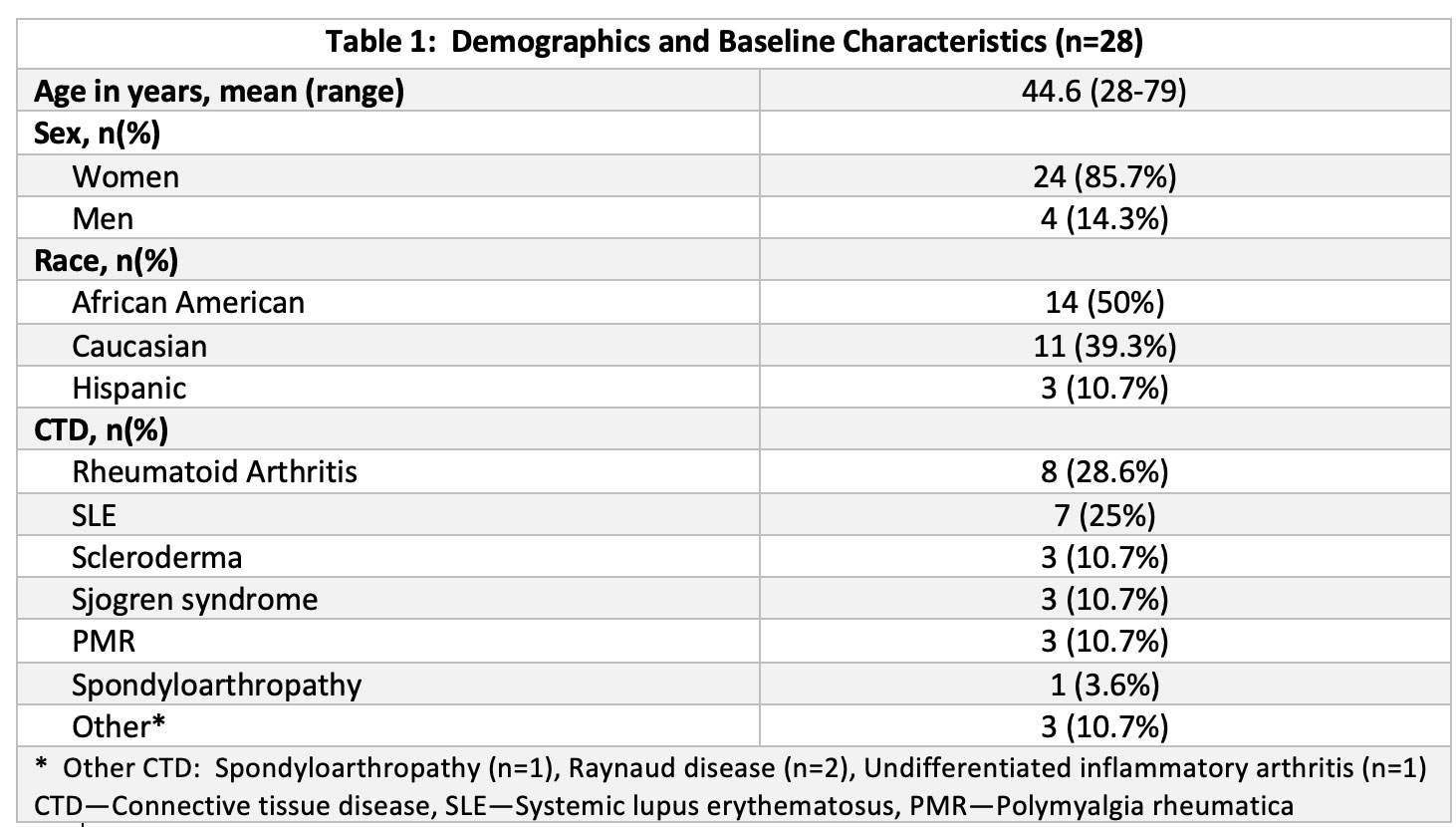
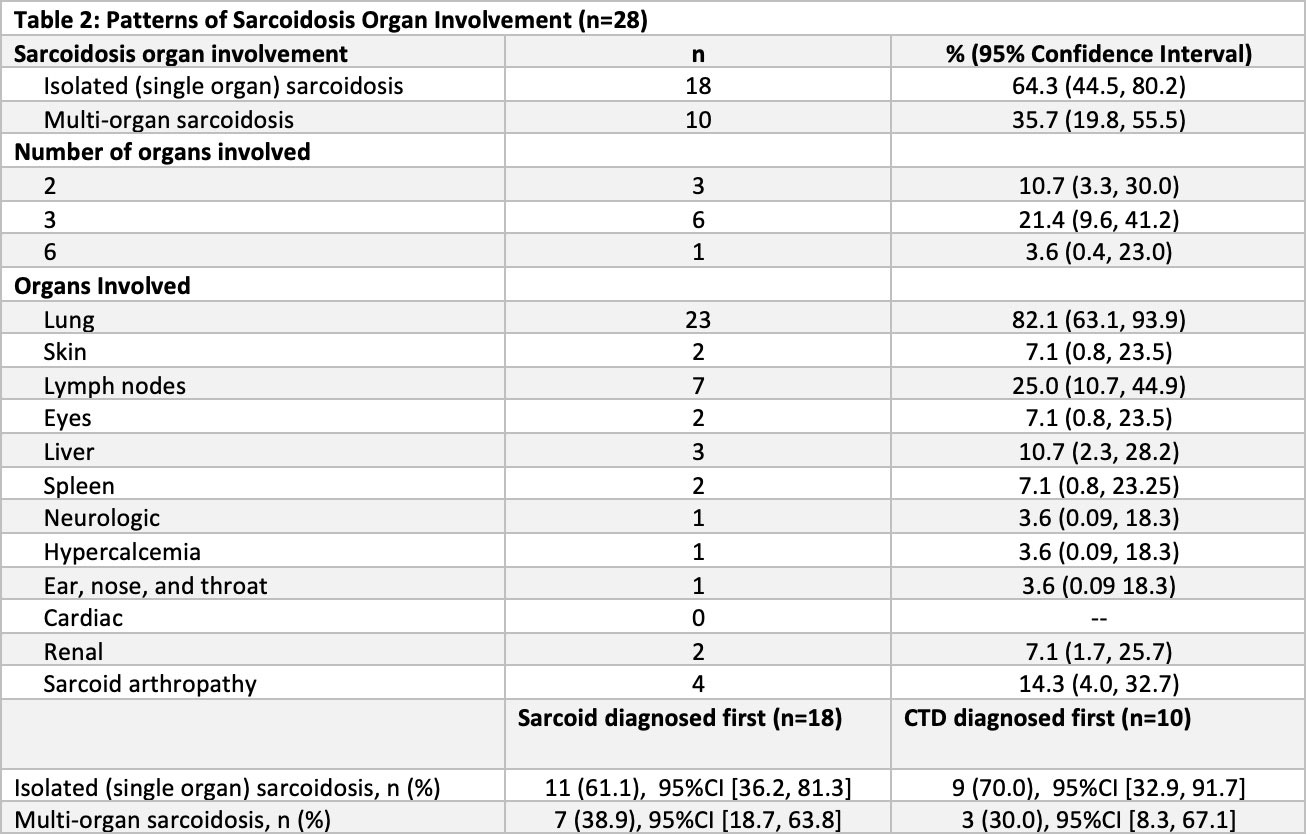
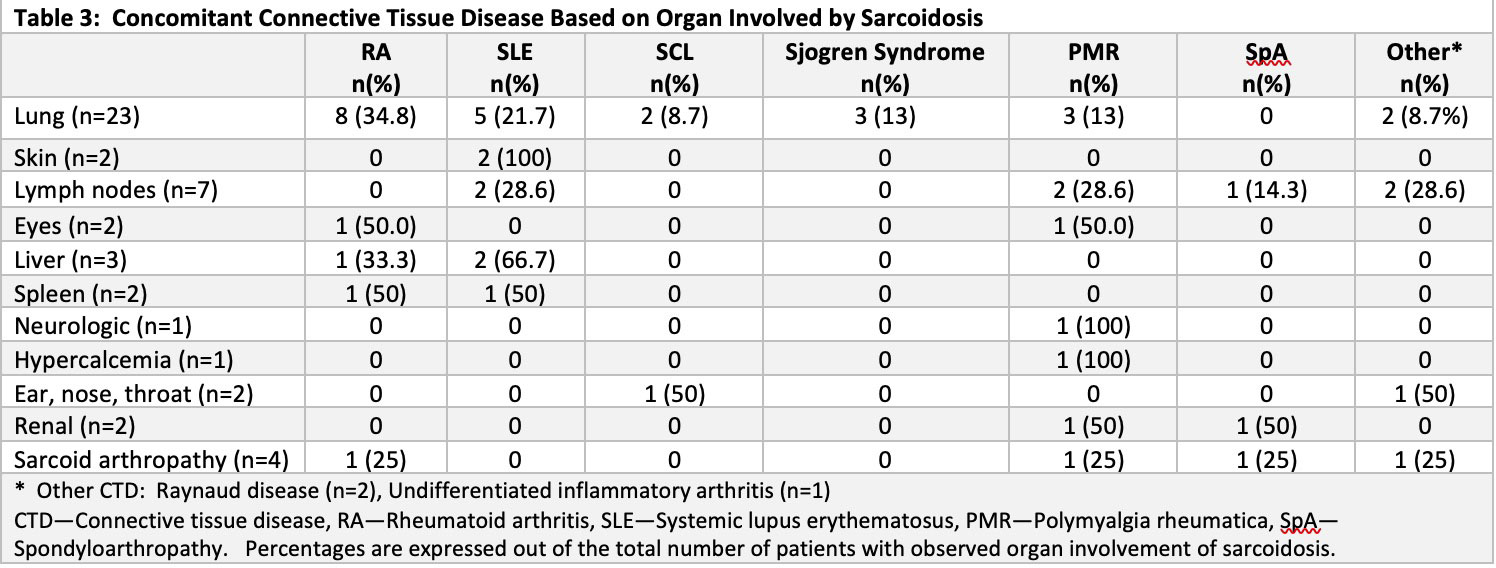
Results: 28 patients were identified with both sarcoidosis and a CTD (Table 1). Patients were more likely to have single organ involvement of sarcoidosis (Table 2) and were diagnosed with sarcoidosis prior to developing CTD (n=18, 60.7%). In these patients, CTD was diagnosed an average of 16 [13 – 20] years later. The 10 patients who developed CTD first were diagnosed with sarcoidosis 6 [4 – 8] years after CTD. The most common coexisting CTD was RA, followed by SLE (Table 1). Patients diagnosed with sarcoidosis before CTD were more likely to develop RA (33.3%), while patients whose CTD developed first were equally likely to have RA or SLE (20%). Patients who developed CTD first were less likely to be in remission when sarcoid was diagnosed (14.3%) despite 85% being on treatment for their CTD at the time of sarcoid diagnosis, compared to 25% of patients who had sarcoid first.
Conclusion: This is the largest study to date of patients with concomitant sarcoidosis and CTD. The majority of this group was female and African American, and the most common CTDs were RA and SLE. A prior case series found that the majority of patients with single organ sarcoidosis were diagnosed with sarcoidosis after their diagnosis of CTD, suggesting that the granulomatous formation was a response to the CTD rather than true sarcoidosis2. This is similar to granulomatous reactions seen in response to some malignancies. This theory is also supported by our observation that patients who had CTD first developed sarcoidosis an average of 6 years later. Interestingly, despite the increased recognition of cardiac sarcoid due to improved imaging techniques, we did not identify any cardiac sarcoid patients in our cohort.
Despite the size of our cohort, larger studies are needed to confirm these findings. Here, we describe characteristics of patients with concomitant sarcoidosis and CTD. Physicians should be aware of this association when caring for patients with sarcoidosis or CTD who later develop findings suggestive of concomitant disease.
1. Baughman RP et al. Ann Am Thorac Soc 2016; 13: 1244–1252
2.Judson MA et al. Respir Med 2013;107:1453-9
To cite this abstract in AMA style:
Harasimowicz M, GIlbert E, Yi S, Ostrowski R. Clinical Features of Patients with Sarcoidosis and Concomitant Connective Tissue Disease [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/clinical-features-of-patients-with-sarcoidosis-and-concomitant-connective-tissue-disease/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/clinical-features-of-patients-with-sarcoidosis-and-concomitant-connective-tissue-disease/