Session Information
Session Type: Poster Session B
Session Time: 9:00AM-10:30AM
Background/Purpose: Pulmonary arterial hypertension (PAH) and interstitial lung disease (ILD) are the leading causes of systemic sclerosis (SSc) associated death. There is increasing interest in the prognosis and outcome of patients who develop both PAH and ILD. We aimed to describe the clinical phenotype and prognosis of people within the Australian Scleroderma Cohort Study (ASCS) with concurrent PAH and ILD.
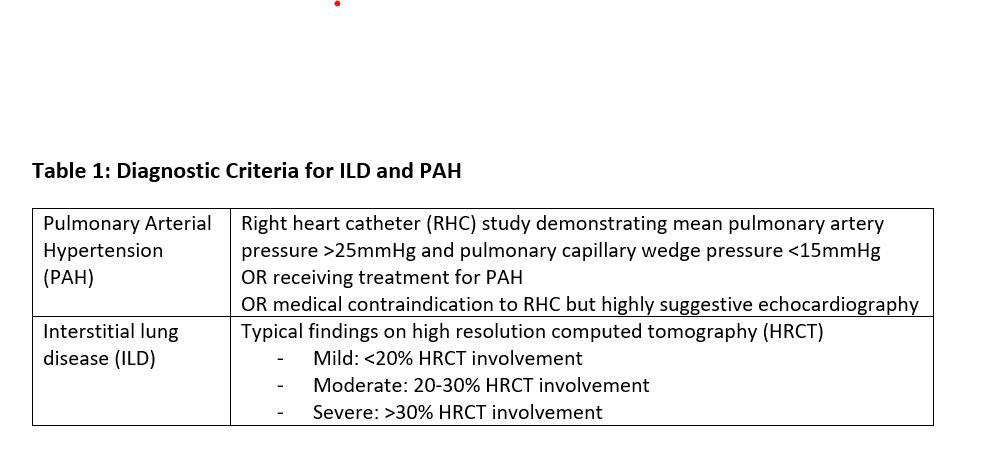
Methods: All ASCS participants meeting ACR/EULAR criteria for SSc were included. Participants were divided into four mutually exclusive groups: those meeting criteria for PAH (Table 1; PAH only group), ILD (Table 1; ILD only group), concurrent PAH and ILD (PAH-ILD group) and neither PAH nor ILD (SSc only group). Associations between demographic and clinical features, health related quality of life and functional status were evaluated using logistic and linear regression. Survival analysis was performed using Kaplan-Meier survival estimates and Cox regression modelling.
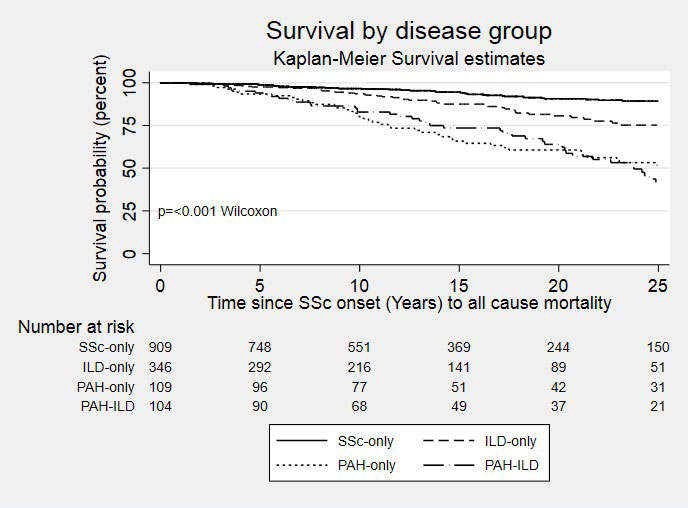
Results: Of 1561 participants, 106 (7%) fulfilled criteria for PAH-ILD, 112 (7%) had PAH only, 373 (24%) had ILD only, and 970 (62%) had SSc only. Participants with ILD were more likely to have diffuse SSc, younger age, Asian background and be non-smokers than those with PAH (p< 0.01). Patients with PAH-ILD or PAH only had worse WHO functional class (Class III/IV PAH-ILD 91.2%, PAH only 85.8% vs ILD only 36.9%, SSc only 15%) and 6-minute walk distance (PAH-ILD 280m, PAH only 296m vs ILD only 444m, SSc only 465m, p< 0.01) than those with ILD only. SF-36 physical component scores were best (highest) in those with no PAH or ILD (p< 0.01) but there was no difference in mental component scores between groups (p=0.79). SSc Health Assessment Questionnaire (SHAQ) scores were worst (highest) in those with PAH-ILD (p< 0.01). Reflux was most common in those with ILD only (86% vs SSc only 81%, PAH ILD 79% and PAH only 74%, p=0.02). Synovitis was most common in PAH-ILD (PAH-ILD 33%, ILD only 30%, SSc only 28% vs. PAH only 21%, p< 0.01), while myositis was most common in those with ILD (ILD only 4.6%, PAH-ILD 4% vs SSc only 2%, PAH only 0.8%, p=0.01). Those with ILD were more likely to have received immunosuppression including prednisolone (PAH-ILD 65%, ILD only 60% vs. SSc-only 37%, PAH only 27%, p< 0.01). Survival was significantly worse in those with PAH or PAH-ILD (p< 0.01 Figure 1). In a multivariable hazard model stratifying ILD by severity (Table 2), severe ILD combined with PAH conferred the worst prognosis (HR = 5.48 95% CI 3.37-8.91 p< 0.01), followed by those with PAH only (HR = 4.22 95% CI 2.89-6.14 p< 0.01) and those with PAH and mild ILD (HR = 2.42 95% CI 2.89-6.14 p< 0.01). Other significant risk factors for mortality were previous renal crisis and longer duration of disease, while factors protective against mortality included centromere-ANA and female sex.
Conclusion: The prevalence of SSc PAH-ILD in the ASCS is 7%, with significant differences in clinical features and worse survival in those with PAH-ILD compared to those with PAH or ILD alone. Further data are required to better understand this high-risk patient group and determine optimal treatments.
Abbreviations: ANA – antinuclear antibody, ILD – interstitial lung disease, PAH – pulmonary arterial hypertension.
To cite this abstract in AMA style:
Fairley J, Hansen D, Ross L, Proudman S, Sahhar J, Ngian G, Walker J, Host L, Morrisroe K, Apostolopoulos D, Ferdowsi N, Wilson M, Tabesh M, Stevens W, Nikpour M. Clinical Characteristics and Survival of Combined Pulmonary Arterial Hypertension and Interstitial Lung Disease in Systemic Sclerosis [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/clinical-characteristics-and-survival-of-combined-pulmonary-arterial-hypertension-and-interstitial-lung-disease-in-systemic-sclerosis/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/clinical-characteristics-and-survival-of-combined-pulmonary-arterial-hypertension-and-interstitial-lung-disease-in-systemic-sclerosis/