Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Hydralazine-induced ANCA-associated vasculitis (HIAAV) is a rare clinical problem. There is paucity of data regarding clinical features, treatment, and prognosis of hydralazine-induced AAV in the literature. In this study, we aimed to evaluate the clinical characteristics and outcomes of HIAAV at our tertiary care center.
Methods: A retrospective chart review was performed from 2014 to 2024. Clinical and laboratory data were extracted from patients’ EMR records. Twenty-two idiopathic AAV patients were included as a control from our hospital. Chi-square and independent t-tests were used to compare categorial and numerical variables between the two groups respectively.
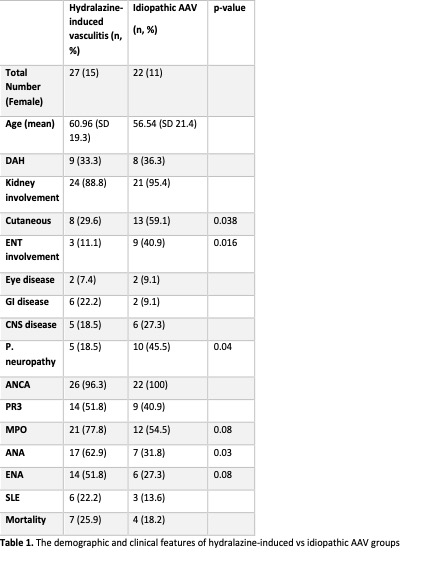
Results: Table 1 summarizes the clinical characteristics of HIAAV and idiopathic AAV patients. We identified 27 patients with HIAAV, of which 55.6% were females. The duration of hydralazine treatment was < 1 year in 5 patients and > 5 years in 8 patients. The most common clinical manifestations of HIAAV were glomerulonephritis (88.8%), diffuse alveolar hemorrhage (33.3%), and cutaneous vasculitis (29.6%). Clinical diagnosis of SLE was prevalent in 22.2% of patients. MPO positivity was more frequent than PR3 in patients with HIAAV (77.8 vs. 51.8%) while dual positivity was recorded in 22.2% of patients. Positive ANA and any kind of positive ENA were also common in HIAVV (62.9% and 63.6%). In this group, drug-induced lupus was also diagnosed in 6 cases with HIAAV. Drug discontinuation was inadequate in most patients with prednisone monotherapy for induction. Rituximab was required in 55.5% patients and Cyclophosphamide in 29.6% patients. PLEX was also used in 11.1% patients. ESRD developed in 37.0% patients with HIAAV and 25.9% patients died. When compared to idiopathic AAV, the frequency of cutaneous vasculitis was 29.6% vs 59.1% (p< 0.05), ENT involvement, 11.1% vs 40.9% (p< 0.05) and peripheral neuropathy, 18.5% vs 45.5% (p< 0.05). ANA positivity was more frequent in the HIAAV group, 62.9% vs. 31.8% (p< 0.05). There was a trend toward MPO positivity with any type of ENA in HIAAV group (p=0.08).
Conclusion: While the most common manifestations in HIAAV were renal, one third had concomitant pulmonary involvement with DAH. Cutaneous, ENT and peripheral neuropathy involvement was more common in idiopathic AAV. Positive ANA and drug-induced-lupus like clinical features were relatively more common in HIAAV group. The study concludes that HIAAV is not a benign condition and may lead to severe morbidity and mortality.
To cite this abstract in AMA style:
Shamim M, Allouni M, Chaudhary H, Daoud A, Dweik L, Syed H, Pamuk O. Clinical Characteristics and Outcomes of Hydralazine-induced ANCA-associated Vasculitis. a Single Center Retrospective Cohort Analysis from the US [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/clinical-characteristics-and-outcomes-of-hydralazine-induced-anca-associated-vasculitis-a-single-center-retrospective-cohort-analysis-from-the-us/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/clinical-characteristics-and-outcomes-of-hydralazine-induced-anca-associated-vasculitis-a-single-center-retrospective-cohort-analysis-from-the-us/