Session Information
Session Type: Poster Session D
Session Time: 1:00PM-3:00PM
Background/Purpose: Post-COVID19 syndrome has been defined as the persistence of symptoms and/or organic damage for more than three weeks after the presence of clinical infection caused by SARS-CoV-2. It is further divided into two categories: subacute and chronic post-COVID19 syndrome. A model that includes clinical, immunological, and metabolic factors regarding this phenomenon have not been fully addressed so far, which is the aim of the present study.
Methods: A cohort study was conducted including 51 patients diagnosed with SARS-CoV-2 infection by RT-PCR and with at least 3 weeks since the onset of symptoms or from hospital discharge. A clinical history was made along with a complete physical examination and routine laboratories and the application of a standardized questionnaire for the detection of symptoms associated with post-COVID19 syndrome. This was repeated 12 months afterwards for detection of chronic post-COVID19. Immunophenotyping of PBMCs by flow cytometry and serum samples were assessed for cytokines, NETs, TRIM63 anti-cellular and anti-SARS-CoV-2 IgG antibodies. Finally, untargeted metabolomics analysis of sera employing gas chromatography coupled to mass spectrometry (GC/MS) was performed. Quantitative variables were expressed as medians and interquartile range. The difference between medians was evaluated using the Mann-Whitney U test. Logistic regression analysis was performed for the presence of Post-COVID19 Syndrome.
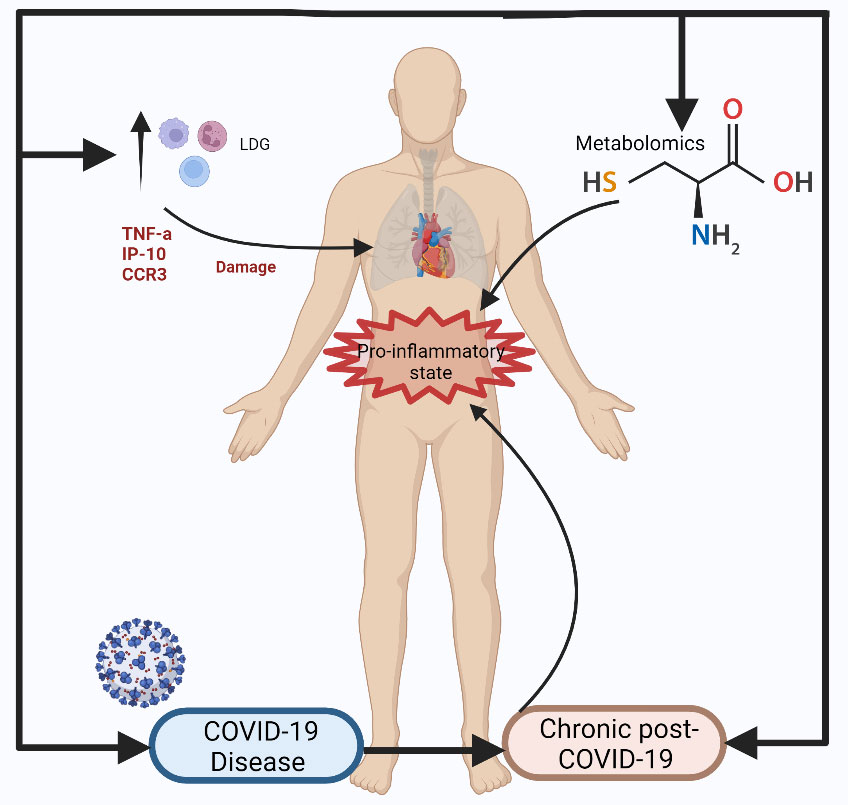
Results: 51 patients were included in the study. 32(62.7%) were men and 19 (37.3%) women with a median age of 48 (24-68) years. 18 (35.2%) met the definition of post-COVID19 syndrome, presenting fatigue as a key symptom. Such patients showed an immunological profile characterized by an increased level of TNF-α (p=< 0.01), IP10 (p=< 0.01), IL-1R (p=< 0.01), CCR3 (p=< 0.05), and increased levels of immature LDGsCD10- (p=< 0.01). Metabolomic levels of α-Hydroxybutyric acid (p=< 0.01), 3,4-dihydroxybutanoic acid (p=< 0.01) and cysteine (p=< 0.01) were associated with the presence of post-COVID19 syndrome.
Conclusion: Our data suggest an important relationship between a pro-inflammatory state mediated through the damage exacerbated during acute COVID19 infection, promoted by an enhanced recruitment of immature granulocytes in an environment enriched with key proinflammatory cytokines in chronic post-COVID-19 syndrome pathophysiology. This could lead to repercussions on the cellular metabolism due to possible alterations derived from hypoxia (metabolism of branched-chain amino acids) and possible redox mechanisms (cysteine/cystine).
To cite this abstract in AMA style:
Camacho-Morán E, torres-Ruiz j, Lira-Luna J, Vargas-Castro A, Pérez-Fragoso A, Nuñez-Aguirre M, Alcalá-Carmona B, Absalón-Aguilar A, Gómez-Martín D. Clinical and Immunological Factors Associated with Chronic Post-COVID19 Syndrome 12 Months After Acute Infection [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/clinical-and-immunological-factors-associated-with-chronic-post-covid19-syndrome-12-months-after-acute-infection/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/clinical-and-immunological-factors-associated-with-chronic-post-covid19-syndrome-12-months-after-acute-infection/