Session Information
Date: Monday, November 9, 2015
Title: Systemic Sclerosis, Fibrosing Syndromes and Raynaud's - Clinical Aspects and Therapeutics Poster II
Session Type: ACR Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose:
Microparticles
(MPs) are membrane-bound vesicles derived from vascular and intravascular cells
such as endothelial cells (EMPs) and platelets (PMPs). Circulating MPs levels
are altered in autoimmune rheumatic diseases (AIRDs) and may act as a
diagnostic and prognostic biomarker, but their precise functional role remains
to be elucidated. We investigated EMP and PMP numbers across a spectrum of
AIRDs with the aim of comparing the levels of, and relationship between, EMPs
and PMPs.
Methods:
Patients with
Systemic Lupus Erythematosus (SLE) (n=24), Systemic Sclerosis (SSc) (n=24),
Primary Raynauds Phenomenon(RP) (n=17) and “other CTD” (n=15) (Primary Sjogrens
Syndrome, UCTD or MCTD ) as well as 15 healthy controls were recruited. Plasma
levels of EMPs (AnnexinV+/CD31+/CD42b-) and PMPs (AnnexinV+/CD31+/CD42b+ or
AnnexinV+/CD31-/CD42b+) were quantified using flow cytometry.
Results:
Patients with SLE
had significantly higher EMPs compared with healthy controls and SSc patients
[(SLE vs health 293,889/ml vs 132,171/ml, p = 0.03), (SLE vs SSc 293,889/ml vs
161,271/ml, p = 0.04)]. In contrast significantly higher PMP levels were noted
in SSc and primary RP when compared to healthy controls and patients in the
other CTD cohort [(SSc vs health 186,348/ml vs 41,085/ml, p < 0.001), (SSc
vs other CTD 186,348/ml vs 58,178/ml, p < 0.001)]. No significant difference
was observed in PMP levels between SLE patients and those with SSc/RP.
A modest
correlation was noted between EMP and PMP levels in health (Spearman r = 0.6, p
= 0.017). This relationship appeared stronger in SLE (Spearman r = 0.72, p <
0.0001) and other CTD patients (Spearman r = 0.75, p < 0.0001). The
association between EMPs and PMPs was notably less strong in SSc (Spearman r =
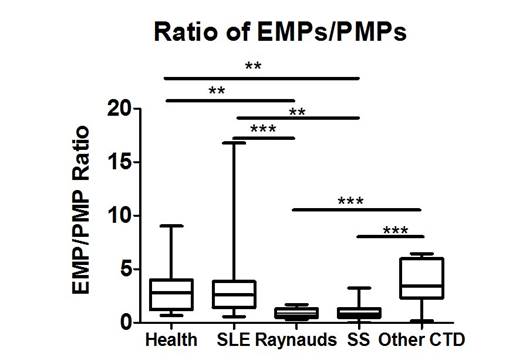
0.45, p = 0.014) and RP (Spearman r = 0.37, p= 0.15). A significantly lower
EMP/PMP ratio was seen in SSc/RP patients in comparison to both healthy
controls and SLE/other CTD patients (Figure 1). Improved disease control,
following alteration in immunosuppressive therapy, was associated with a
reduction in EMP and PMP numbers in SLE, a result that was significant for PMPs
(75,969/ml vs 32,171/ml, p = 0.02). In contrast, the addition of Asasantin in
SSc/primary RP patients did not affect MP levels at follow up.
Conclusion:
MP populations
differ across the spectrum of AIRDS, with high PMPs seen in SSc/RP and high
EMPs observed in SLE. The ratio of EMPs/PMPs appears to distinguish between
SLE/other CTD and SSc/primary RP, suggesting differential production of MPs
according to the vascular pathology and bed involved. Improved disease control
reduces PMP levels in SLE, but antiplatelet agents do not materially affect MP
numbers in SSc/RP. MPs may therefore act as diagnostic and prognostic biomarkers
in AIRDs.
Figure 1. The ratio of EMPs/PMPs
in SLE, primary Raynauds, Systemic Sclerosis and other CTD patients.
To cite this abstract in AMA style:
McCarthy EM, Moreno-Martinez D, Wilkinson F, McHugh NJ, Bruce IN, Alexander Y, Pauling JD, Parker B. Circulating Microparticle Populations May Differentiate Between Connective Tissue Diseases. [abstract]. Arthritis Rheumatol. 2015; 67 (suppl 10). https://acrabstracts.org/abstract/circulating-microparticle-populations-may-differentiate-between-connective-tissue-diseases/. Accessed .« Back to 2015 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/circulating-microparticle-populations-may-differentiate-between-connective-tissue-diseases/