Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
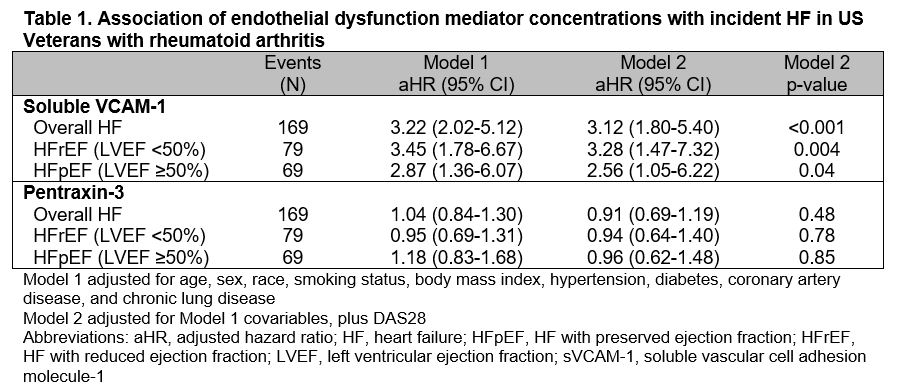
Background/Purpose: Endothelial dysfunction, leading to myocardial inflammation and dysfunction, may drive a heightened risk of heart failure (HF) in people with rheumatoid arthritis (RA). Circulating mediators of endothelial dysfunction (soluble vascular cell adhesion molecule-1 [sVCAM-1] and pentraxin-3) that predict HF development in non-RA populations are upregulated in RA; however, their influence on HF development in RA is unknown. We examined these analytes as predictors of incident HF and HF subtypes, independent of RA disease activity.
Methods: In a multicenter, prospective cohort of US Veterans with RA, pentraxin-3 and sVCAM-1 were measured from banked serum at enrollment. Analyte concentrations were log-transformed, standardized, and categorized into quartiles. Incident HF was defined as the first HF hospitalization or HF-related death after enrollment, using validated administrative algorithms in linked VA, Medicare, and National Death Index data. Left ventricular ejection fraction (LVEF) values were extracted from clinical notes through a validated natural language processing tool, and HF subtypes (HF with reduced EF [HFrEF] < 50%, HF with preserved EF [HFpEF] ≥50%) were defined by the most proximate LVEF within 1 year prior to a HF event, or if missing, < 30 days following the event. Participants free of HF were followed to incident HF, death, or end of study period (01/2020). Cox regression was used to test the association of sVCAM-1 and pentraxin-3 concentrations with incident HF, adjusting for traditional cardiovascular (CV) risk factors and RA disease activity (DAS28). We tested the dose-dependent relationship of analyte quartiles with incident HF risk in similar Cox regression models, stratified by DAS28 categories.
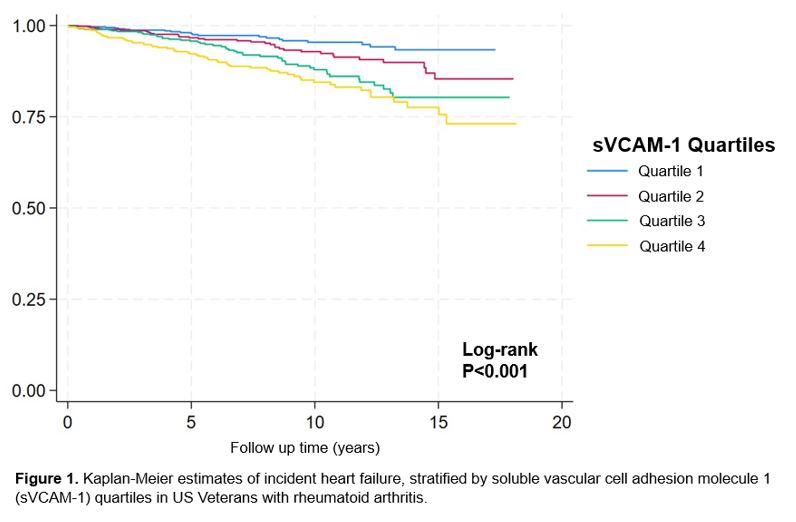
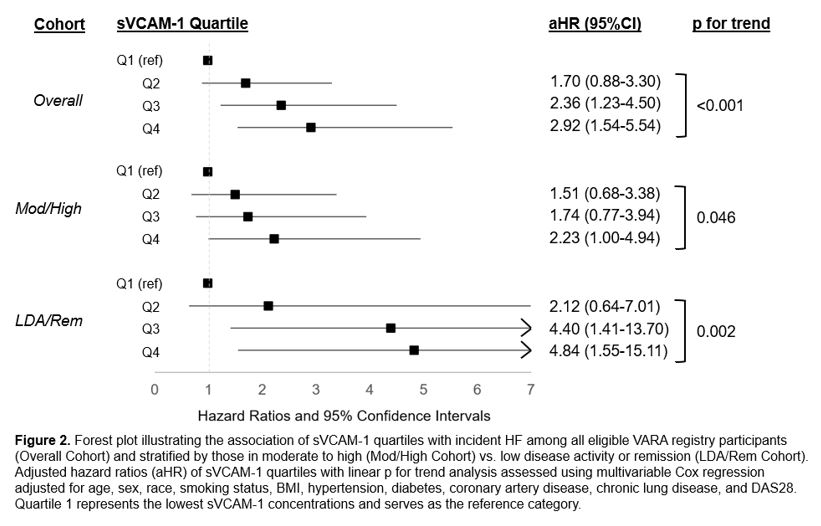
Results: Among 2,271 participants (mean age 64 years, 87% male, mean DAS28 3.6) free of HF at baseline, 169 incident HF events occurred over a median follow up of 6.9 years. Mean pentraxin-3 (p< 0.01), but not sVCAM-1 (p=0.11) concentration was higher in those with moderate to high DAS28. After adjustment for demographics and traditional CVD risk factors, sVCAM-1 concentration was associated with an increased risk of incident HF (Table 1; per SD aHR 3.22 [2.02-5.12]), which persisted after additional adjustment for DAS28 (aHR 3.12 [1.80-5.40]). Associations between sVCAM-1 with HFrEF (aHR 3.28 [1.47-7.32]) and HFpEF (aHR 2.56 [1.05-6.22]) were similar. Survival worsened (Figure 1; log-rank p< 0.001) and strength of association with incident HF increased among higher quartiles of sVCAM-1 (Figure 2; Q4 vs. Q1 aHR 2.92 [1.54-5.54]; p for trend < 0.001). Patterns were similar after stratification by moderate or high (p for trend = 0.046) vs. low RA disease activity or remission (p for trend = 0.002). Pentraxin-3 was not associated with incident HF or HF subtypes (range aHR 0.91-0.96).
Conclusion: In a large, prospective RA cohort, sVCAM-1 concentrations were associated with a dose-dependent increase in the risk of incident HF, independent of traditional CV risk factors and RA disease activity. These findings implicate endothelial dysfunction as an independent risk factor for HF in RA and may inform research into targeted prediction and management strategies to prevent HF development in RA.
To cite this abstract in AMA style:
Johnson T, Duryee M, Hunter C, Roul P, Baker J, Cannon g, Wallace B, Monach P, Reimold A, Kerr G, Smith I, Richards J, Wysham K, Kunkel G, Lee I, Anderson D, Thiele G, Mikuls T, England B. Circulating Mediators of Endothelial Dysfunction as Predictors of Incident Heart Failure in Rheumatoid Arthritis [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/circulating-mediators-of-endothelial-dysfunction-as-predictors-of-incident-heart-failure-in-rheumatoid-arthritis/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/circulating-mediators-of-endothelial-dysfunction-as-predictors-of-incident-heart-failure-in-rheumatoid-arthritis/