Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Sjögren’s syndrome (SS) is a chronic autoimmune disorder primarily affecting the exocrine glands, but it also impacts various parts of the respiratory system, including the oropharynx, the trachea, and the distal lung parenchyma, often manifesting as interstitial lung disease. The unified airway hypothesis in asthma suggests that upper and lower airway diseases are part of a single pathological continuum. Further, in various autoimmune diseases, such as eosinophilic granulomatosis with Polyangiitis (EGPA) and granulomatosis with polyangiitis (GPA), upper airway disease often precedes the development of lower airway disease. With this in mind, this study tested the hypothesis that chronic sinus disease may predict the development of lower airways in SS, specifically interstitial lung disease.
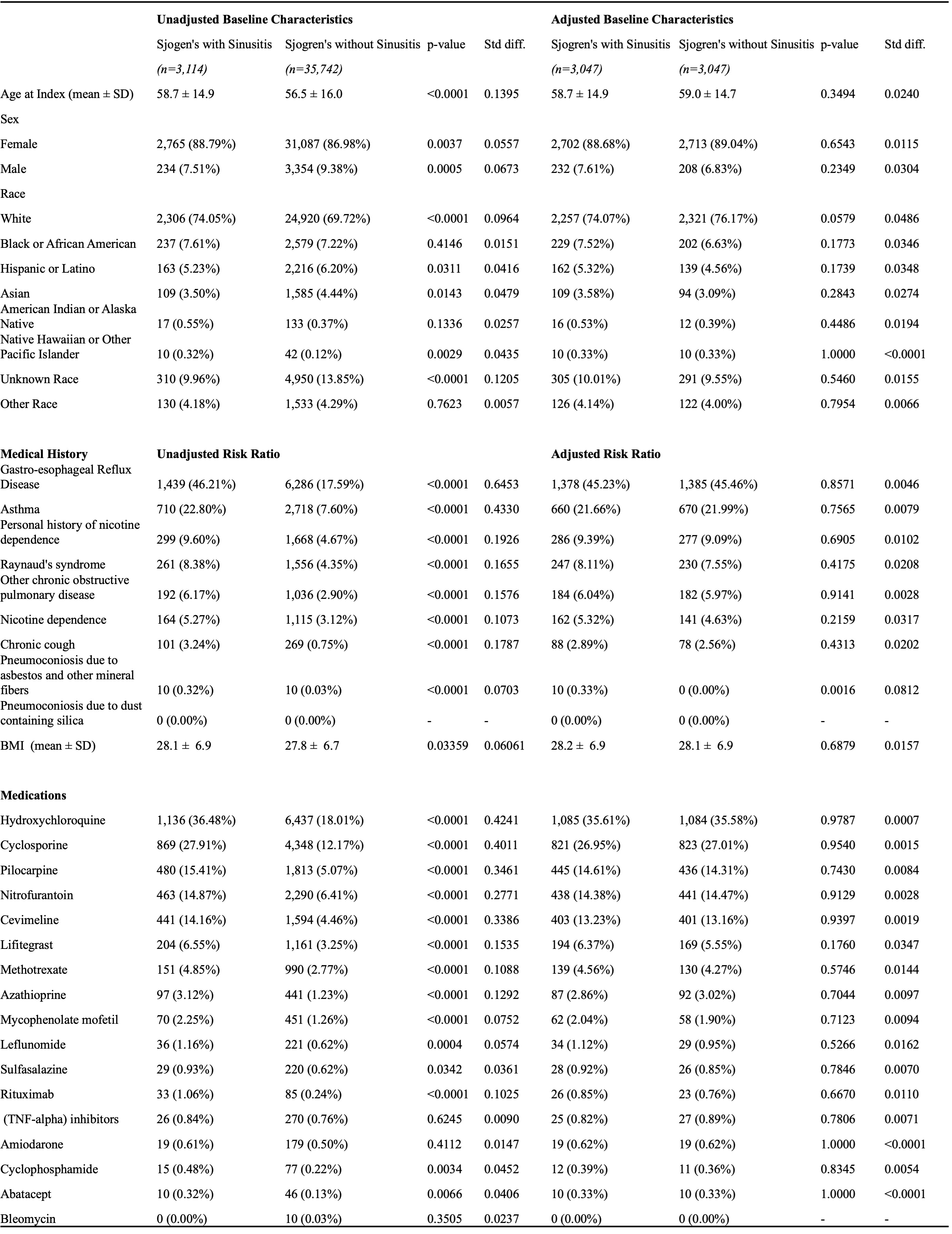
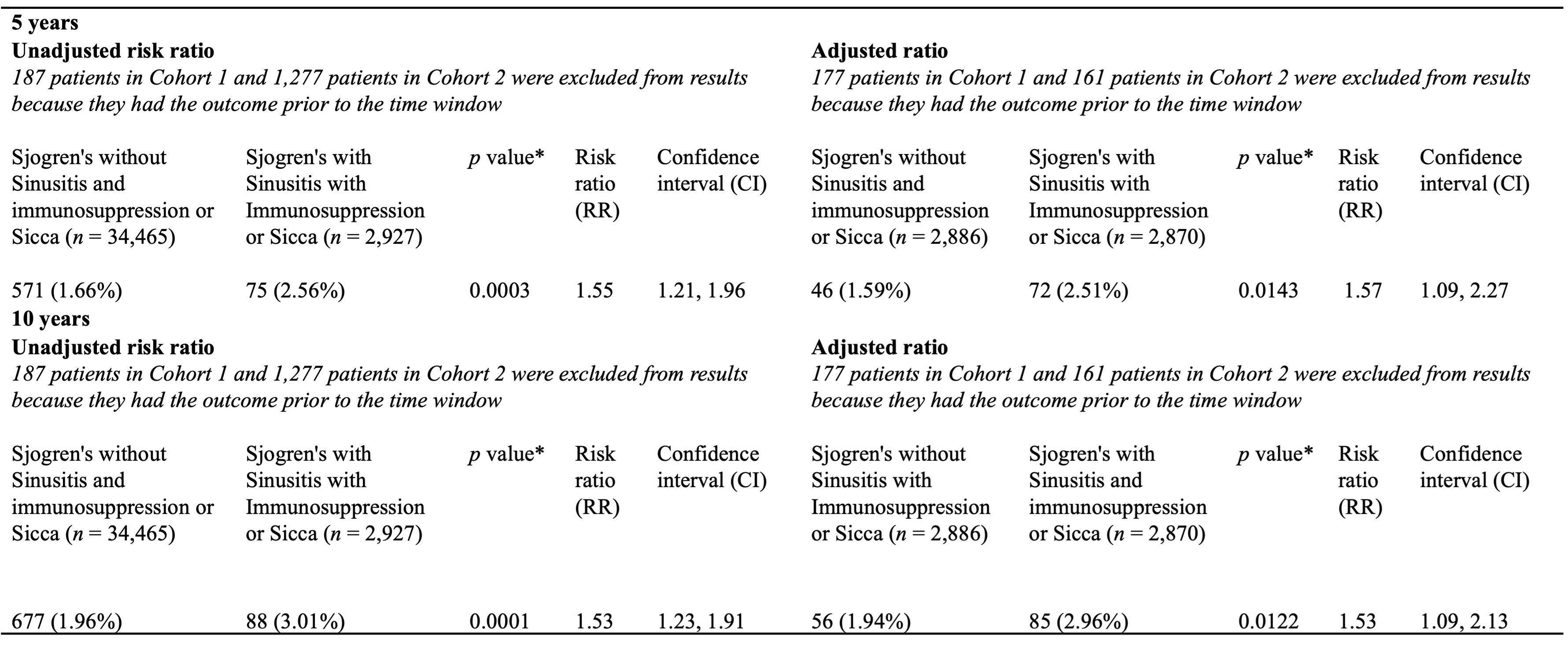
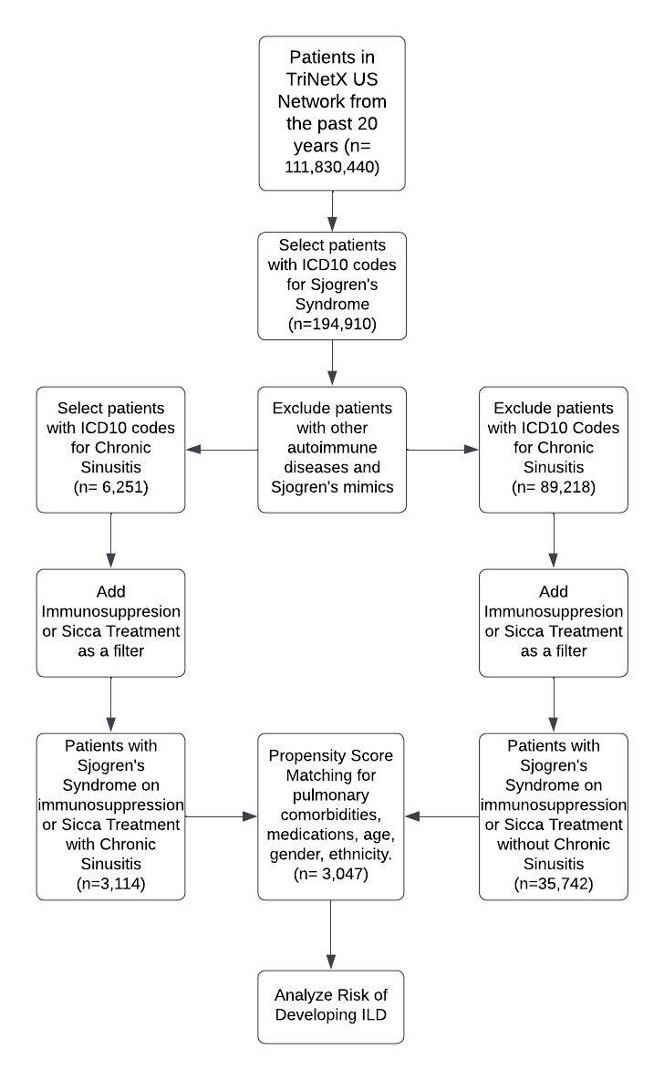
Methods: Using the TriNetX Research Network’s de-identified electronic health records, this study utilized data from 61 U.S. healthcare networks from 2004 to 2024. Two cohorts were established: patients with SS followed by a diagnosis of chronic rhinosinusitis (CRS) and patients with SS without CRS. At the time of study inclusion, patients had an ICD-9 or ICD-10 code for SS and received immunosuppressive medications or treatments for ocular or mucocutaneous dryness. Patients with other autoimmune diseases and conditions mimicking SS were excluded. An association analysis was conducted to calculate the fraction of patients developing ILD and to compare the risk ratio (RR) between the cohorts 5 and 10 years post-CRS diagnosis. Propensity score matching (PSM) was used to adjust for age, sex, race, comorbid pulmonary conditions, and ILD risk factors. The RR was calculated with a 95% confidence interval and a significance level of p< 0.05.
Results: The study included 38,856 patients with SS. The mean age was 58.7 years for the CRS group and 56.5 years for the non-CRS group, with females constituting 88.79% and 86.98% of these groups, respectively. ILD was more prevalent in the CRS group (2.56% at 5 years and 3.01% at 10 years) compared to the non-CRS group (1.66% at 5 years and 1.96% at 10 years). After PSM, adjusted RRs remained significantly higher in the CRS group (2.51% vs. 1.59% at 5 years and 2.96% vs. 1.94% at 10 years), with adjusted RRs of 1.57 (p = 0.0143) at 5 years and 1.53 (p = 0.0122) at 10 years.
Conclusion: Our findings indicate that chronic sinus disease may be a risk factor for the development of lower airway disease in SS, supporting the notion of a disease continuum in this condition. Future studies should further investigate this relationship.
To cite this abstract in AMA style:
Schonewald B, summer R, Loizidis G, Xie C. Chronic Sinusitis Predicting Interstitial Lung Disease in Sjögren’s Syndrome: A Comprehensive USA Population Study (2004-2024) [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/chronic-sinusitis-predicting-interstitial-lung-disease-in-sjogrens-syndrome-a-comprehensive-usa-population-study-2004-2024/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/chronic-sinusitis-predicting-interstitial-lung-disease-in-sjogrens-syndrome-a-comprehensive-usa-population-study-2004-2024/