Session Information
Date: Wednesday, November 8, 2017
Title: Systemic Sclerosis, Fibrosing Syndromes and Raynaud's – Clinical Aspects and Therapeutics III
Session Type: ACR Concurrent Abstract Session
Session Time: 11:00AM-12:30PM
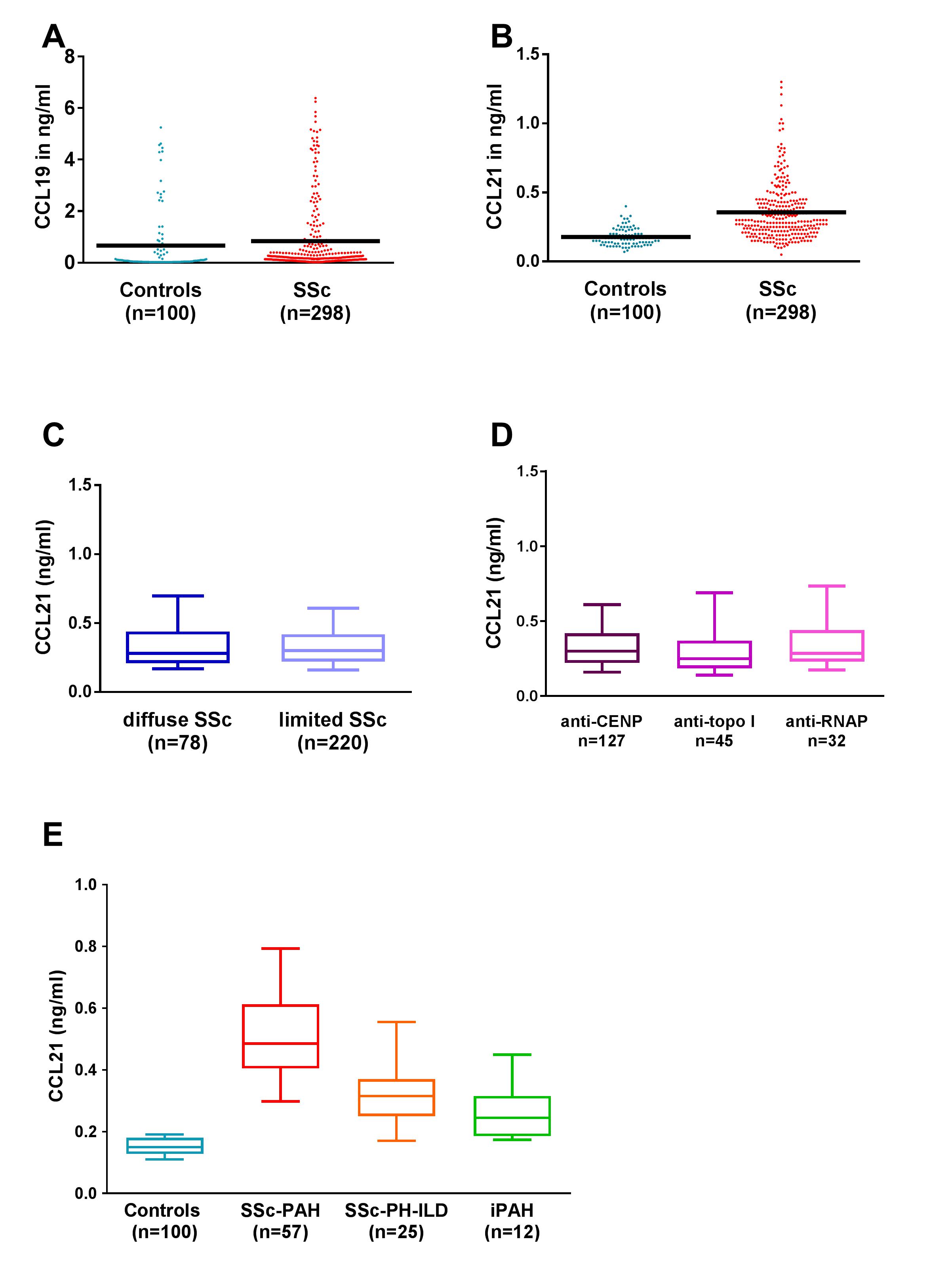
Background/Purpose : Systemic sclerosis (SSc) is a major cause of pulmonary arterial hypertension (PAH). Murine models indicate key roles of chemokines CCL19/21 and their receptor CCR7 in lung inflammation leading to PAH. We aimed to assess the chemokine CCL19/21 axis in SSc-PAH.
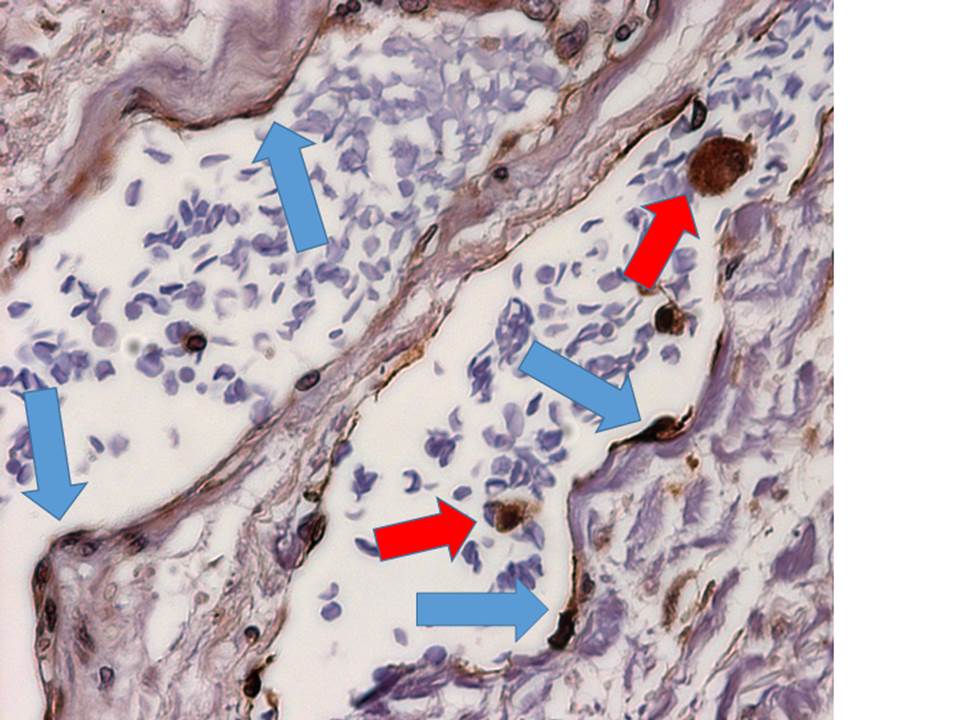
Methods: Sera from two independent prospective SSc cohorts including Oslo University Hospital (OUH, n=298) and Lund University Hospital (LU, n=28), idiopathic PAH (n=12) and controls (n=100) were analysed for CCL19/CCL21 by ELISA. Levels were defined as high or low using [mean + 2SD] in controls as cut-off. Risk stratification at time of PAH diagnosis was performed according to 2016 European Society of Cardiology guidelines. PAH related events were defined as; (a) PAH progression (b) end-stage PAH (c) hospitalization for PAH worsening and (d) all-cause mortality. Cellular sources of CCL21 and CCR7 within SSc-PAH lung tissue were determined by immunohistochemistry.
Results: CCL21 was higher in SSc than controls, and stable across time of PAH diagnosis. Clinical and demographics are shown in Table 1. 129/298 SSc patients underwent RHC at OUH, 41 were diagnosed with PAH and 25 with PH-ILD; at LU 16 patients had PAH. PAH was more frequent in patients with high CCL21 (>0.4 ng/ml) than low CCL21 (33.3% versus 5.3%, p<0.001) and higher than in PH-ILD and idiopathic PH (Figure 1). In multivariate analyses, CCL21 was associated with PAH (HR 5.1 95% CI 2.39-10.76, p<0.001) and predictive for new onset PAH (HR 3.3, 95% CI 1.52-7.10, p=0.003). CCL21 was associated with occurrence of PAH related events (HR 4.7, 95%CI 2.12-10.46, p<0.001). Risk stratification at PAH diagnosis alone did not predict PAH related events, but when combined with CCL21 (HR 1.3, 95% C 1.03-1.60, p=0.027). Survival at 5- and 10-years differed between high and low CLL21 subsets (87% and 71% versus 96% and 91%, p<0.001). Main cellular sources of CCL21 in SSc-PAH lungs were vascular endothelial cells and circulating mononuclear cells (Figure 2), while CCR7 marked infiltrating vascular wall mononuclear cells.
Conclusion: CCL21 appears as a promising marker for SSc-PAH risk prediction and PAH progression. CCL21 may be part of a deregulated immune pathway linked to development of lung vascular damage in SSc.
Table 1:
|
|
Total |
|
SSc-PH |
|
iPAH
|
|
|
|
PAH |
PAH |
PH-ILD |
|
|
|
OUH (n=298) |
OUH (n=41) |
LU† (n=16) |
OUH (n=25) |
OUH (n=12) |
|
Age at onset, yrs |
56 (13.9) |
66.8 (8.2) |
68.6(10.3) |
59.5(10.2) |
40.3(14.5) |
|
Time from onset to PH, yrs |
n.a. |
12.1(10.8) |
15.2 (6.5) |
8.7 (5.6) |
0 (0) |
|
Time from sera sampling to PH, yrs |
n.a. |
-2.1 (3.8) |
-2.6 (0.7) |
-1.4 (2.7) |
0.07 (1.2) |
|
Males, no (%) |
55(18.5) |
9 (22) |
2 (12.5) |
9 (36) |
2 (16.7) |
|
Deceased, no (%) |
99 (31.6) |
21 (51.2) |
11 (68.8) |
15 (60) |
4 (33.3) |
|
Diffuse cutaneous SSc, no (%) |
78 (26.2) |
4 (9.8) |
0 (0) |
6 (24) |
n.a. |
|
Anti-centromere Ab, no (%) |
127(46.9) |
25 (69.4) |
8 (50) |
5 (20) |
n.a. |
|
mPAP at diagnosis, mmHg |
n.a. |
39.1(11.9) |
38.5(10.1) |
36.3(11.6) |
55.1(17.1) |
|
CCL21 at baseline, pg/ml |
|
0.51 (0.2) |
0.60 (0.3) |
0.33 (0.1) |
0.26 (0.1) |
Figure 1:
Figure 2:
To cite this abstract in AMA style:
Hoffmann-Vold AM, Hesselstrand R, Fretheim H, Ueland T, Andreassen AK, Midtvedt O, Garen T, Aukrust P, Belperio JA, Molberg Ø. Chemokine CCL21 As a Potential Serum Biomarker for Pulmonary Arterial Hypertension in Systemic Sclerosis [abstract]. Arthritis Rheumatol. 2017; 69 (suppl 10). https://acrabstracts.org/abstract/chemokine-ccl21-as-a-potential-serum-biomarker-for-pulmonary-arterial-hypertension-in-systemic-sclerosis/. Accessed .« Back to 2017 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/chemokine-ccl21-as-a-potential-serum-biomarker-for-pulmonary-arterial-hypertension-in-systemic-sclerosis/