Session Information
Date: Sunday, November 17, 2024
Title: Muscle Biology, Myositis & Myopathies – Basic & Clinical Science Poster II
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: The aim of this study is to assess if there are clinical and serological differences in patients with idiopathic inflammatory myopathies (IIM) according to multiple versus single positivity myositis specific antibodies (MSA) determined by line immunoassay (LIA). In patients with muscle biopsy, differences between groups were also analyzed.
Methods: We retrospectively reviewed all the patients who satisfy 2017 EULAR/ACR classification criteria for adult and juvenile IIM and who had MSA panel by LIA between March 2023 and May 2024. Due to the number of patients, only anti-Mi2 and anti-TIF1γ were subanalyzed. Chi-square, Fisher’s, Mann-Whitney U and Kruskall Wallis tests were used for association between groups. Two-tail p value < 0.05 was considered statistically significant.
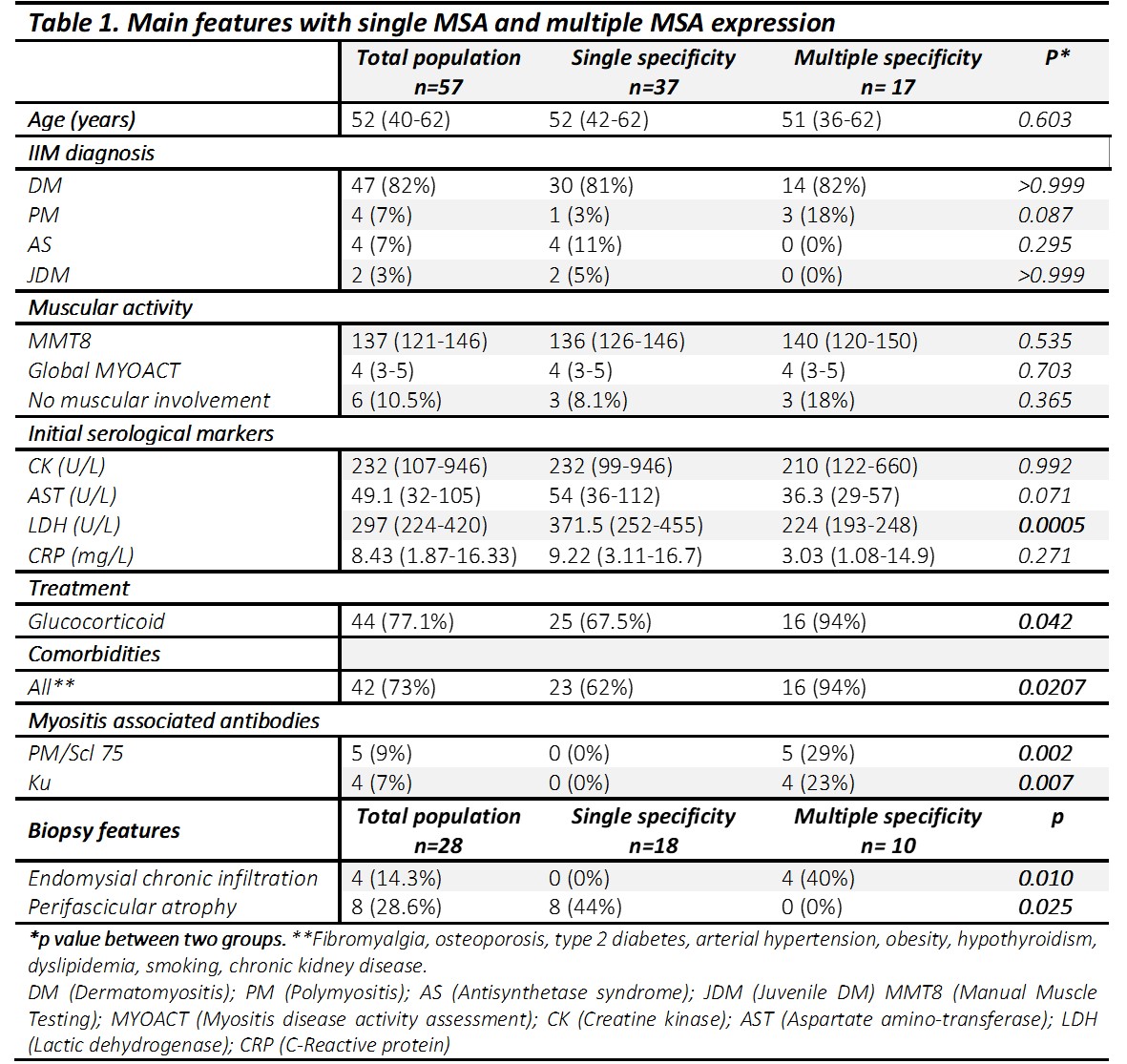
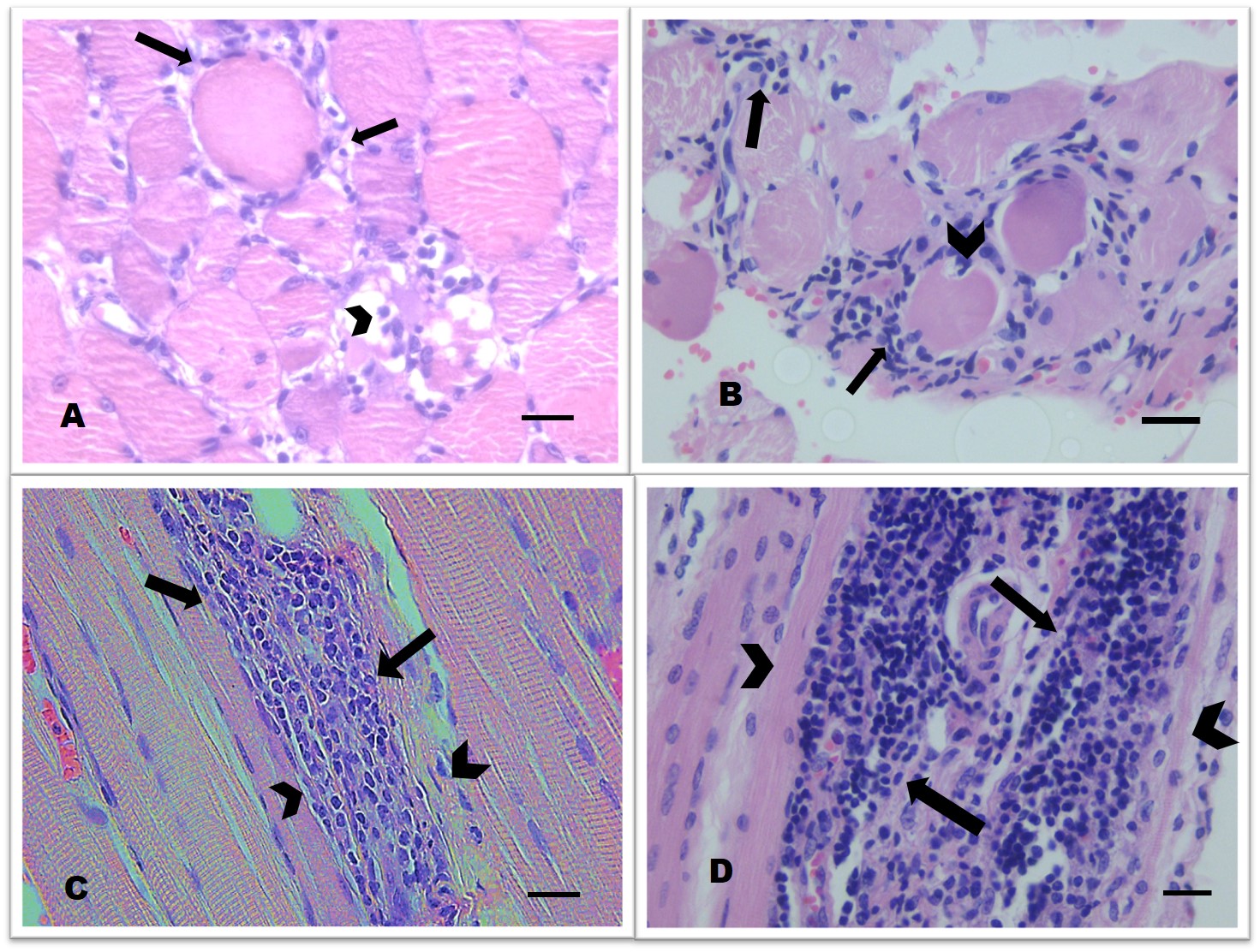
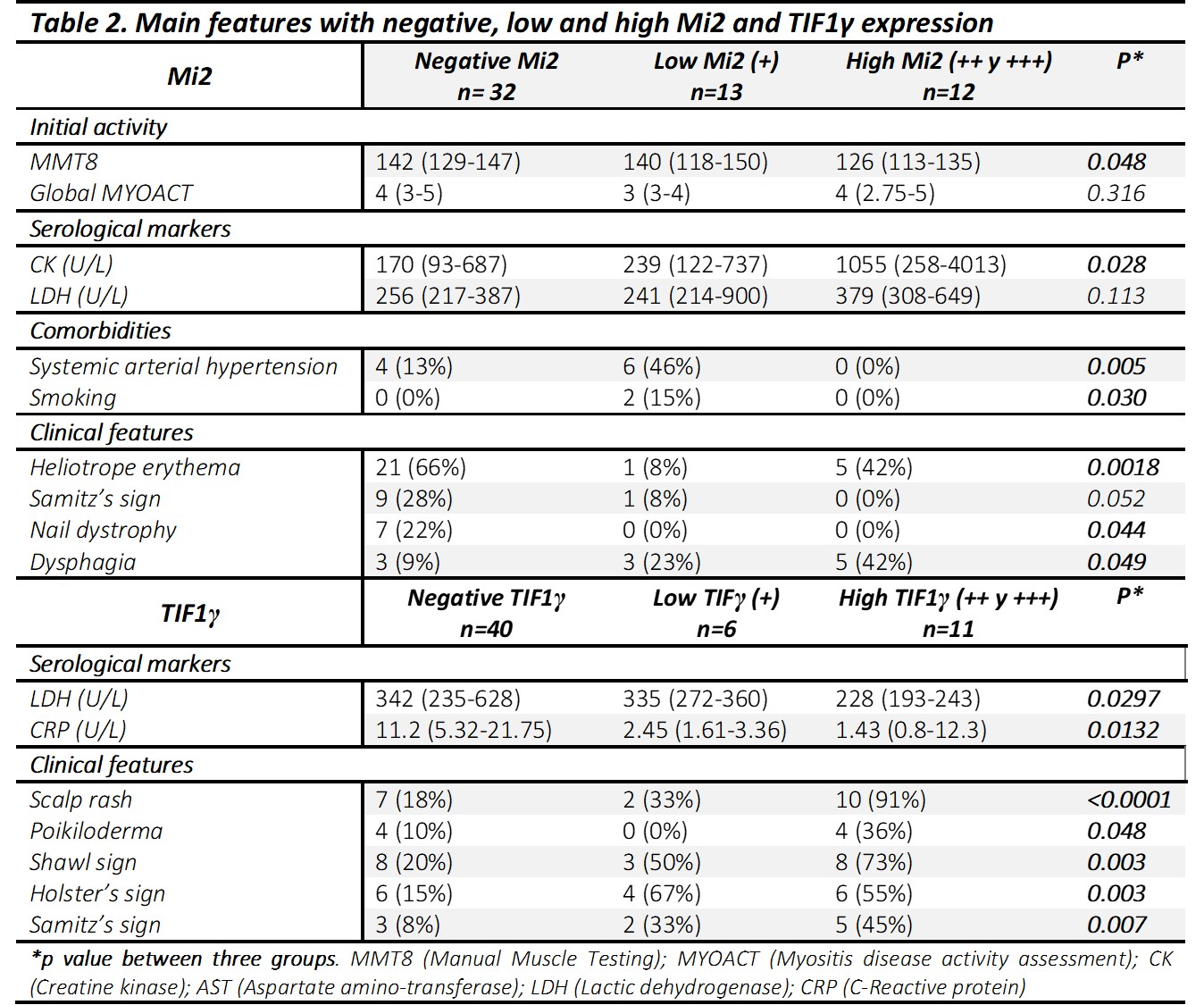
Results: Fifty-seven patients were included; forty-two (73%) female. IIM diagnosis distribution is in table 1. Fifty-four patients (94.7%) had ≥1 MSA; thirty-seven (64.9%) were single MSA positive and 17 (29.8%) multiple. Anti-Mi2 was the most common MSA, it was present in 25 patients (44%), followed by anti-TIF1γ in 17 (30%), anti-MDA5 in 12 (21%), anti-SRP in 9 (16%), anti-SAE in 8 (12%), anti-Jo-1 and anti-PL-7 7 each one (12%), anti-PL-12 in 5 (9%), anti-OJ in 4 (7%), anti-NXP2 and anti-EJ 2 each one (3%). In general, no differences in activity were observed between groups (table 1). Initial LDH levels were higher in patients with single MSA positivity; in those with multiple positivity, the use of prednisone and comorbidities were more frequent. Anti-PM/Scl 75 and anti-Ku were present only in multiple positivity group (table 1). Twenty-eight patients (49.1%) had muscle biopsy available. Perifascicular atrophy was identified in single MSA positivity group, while chronic endomysial infiltrate in multiple positivity (figure 1). Heliotrope rash and nail dystrophy were more frequent in negative anti-Mi2; while positive anti-Mi2 was related with dysphagia. Lower MMT-8 scores and higher creatin kinase levels were observed in high positive anti-Mi2 (table 2). Patients with strongly positive anti-TIF1γ had lower LDH and C reactive protein. Dermatological features were more frequent in stronger positive anti- TIFγ antibodies (table 2); the 6 patients with low positive anti-TIF1y antibodies had hypothyroidism and 2 had breast cancer
Conclusion: Strong positivity by LIA seems to have greater clinical and serological correlations, as anti-Mi2 and anti-TIF1γ in this study. Few differences were found between multiple positivity versus single positivity MSA: glucocorticoid use and comorbidities were more frequent in the former. Presence of anti-PM/Scl 75, anti-Ku and endomysial chronic infiltration was present only in multiple MSA. Studies with more patients are required to evaluate if there are clinical and histological differences in patients with one or multiple MSA, including comparisons with specific tests as ELISA.
To cite this abstract in AMA style:
Miguel-Álvarez A, Amezcua Guerra l, Loredo-Mendoza M, Silveira Torre L, Vargas Guerrero A. Characterization of the Clinical Presentation of Idiopathic Inflammatory Myopathies According to the Profile of Specific Autoantibodies with Multiple Positivity [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/characterization-of-the-clinical-presentation-of-idiopathic-inflammatory-myopathies-according-to-the-profile-of-specific-autoantibodies-with-multiple-positivity/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/characterization-of-the-clinical-presentation-of-idiopathic-inflammatory-myopathies-according-to-the-profile-of-specific-autoantibodies-with-multiple-positivity/