Session Information
Session Type: Poster Session B
Session Time: 5:00PM-6:00PM
Background/Purpose: Given the high prevalence of intestinal lung disease (ILD) in systemic sclerosis (SSc) and the low sensitivity of pulmonary function testing for diagnosing ILD, current guidelines recommend ILD-screening with high resolution computed topography (HRCT) at diagnosis. Although HRCT is critical for appropriate ILD diagnosis and management, these screenings may lead to the discovery of pulmonary nodules, an infrequently described feature of SSc. Unlike adults, incidental pulmonary nodules in children produce a clinical dilemma as there are no evidence-based management guidelines and they rarely represent malignancy. Children with Juvenile-onset SSc (jSSc) have risk factors for pulmonary inflammation and therefore nodule development, such as increased prevalence of esophageal dysfunction (e.g. reflux aspiration), usage of immunosuppression (e.g. infection), and systemic inflammation (e.g. early ILD), although the prevalence of nodules in jSSc is unknown. We sought to evaluate the prevalence and characteristics of pulmonary nodules in jSSc.
Methods: Data was curated in January 2022 from the National Registry for Childhood Onset Scleroderma (IRB PRO11060222), a prospective research registry of patients with jSSc evaluated at a single tertiary care institution with an associated multidisciplinary jSSc clinic. All patients fulfilled the 2013 ACR/EULAR criteria for SSc. Demographic, serologic, radiological, clinical, and laboratory data were extracted. Chest HRCTs and/or reports were reviewed by a pediatric pulmonologist and radiologist. Bivariate analysis was used to compare select measures between children with and without nodules on imaging (significance defined a p < 0.05).
Results: Of 40 children enrolled in the registry, 32 children received a HRCT chest and 15 had reports of nodule(s). Independent review confirmed nodules in 12 (38%) of 32 children. Most had > 1 nodule and at least one follow-up HRCT. Bivariate analysis results are reported in Table 1. Those with nodules were younger at initial imaging, had less time between diagnosis and onset of symptoms, and higher prevalence of sclerodactyly. More children with nodules had ILD and decreased usage of disease-modifying anti-rheumatic drugs compared to children without nodules, although neither was statistically significant. No association with gastrointestinal features were observed. Most nodules were < 5mm in size and stable over time. No nodules were biopsied.
Conclusion: Pulmonary nodules may be a more common pulmonary feature as over one third of jSSc patients in a tertiary referral center registry revealed nodule(s) on HRCT chest. Most nodules were small and demonstrated stability over time. The etiology of the pulmonary nodules is unknown however may be related to systemic inflammation given the association with younger age, earlier symptoms, and sclerodactyly. Larger cohort studies are needed to better characterize the prevalence and natural course of pulmonary nodules in jSSc, including the association with ILD.
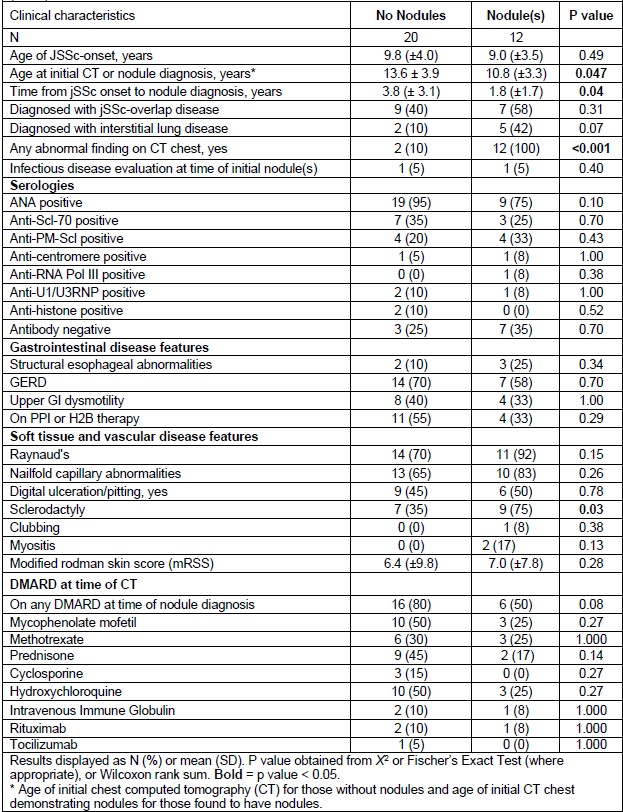 Table 1: Select characteristics of juvenile systemic sclerosis registry participants with at least one CT scan (Nf32)
Table 1: Select characteristics of juvenile systemic sclerosis registry participants with at least one CT scan (Nf32)
To cite this abstract in AMA style:
Li J, Rosser F, Tadros S, Torok K. Characterization of Pulmonary Nodules in Juvenile-onset Systemic Sclerosis: A Single Center Case-Series [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 4). https://acrabstracts.org/abstract/characterization-of-pulmonary-nodules-in-juvenile-onset-systemic-sclerosis-a-single-center-case-series/. Accessed .« Back to 2023 Pediatric Rheumatology Symposium
ACR Meeting Abstracts - https://acrabstracts.org/abstract/characterization-of-pulmonary-nodules-in-juvenile-onset-systemic-sclerosis-a-single-center-case-series/
