Session Information
Date: Monday, October 27, 2025
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: -Sjogren’s syndrome (SS) is a chronic autoimmune disorder, defined by keratoconjunctivitis sicca (KCS), specific serologies, and a significant risk of extra-exocrine disease manifestations and B-cell lymphoma1. – Amyloidosis is the local or systemic accumulation of abnormal protein aggregates2.-Localized amyloidosis is a known, but rare, complication of SS3, and is poorly characterized as to long-term course and treatment options.-We report a case series of eight individuals with SS and localized amyloidosis, followed for an average of 8.65 years (range 1-21 years). Our results were compared to literature review to compile a description of localized amyloidosis in the setting of SS.
Methods: Our eight-patient cohort was seen and followed by PG over a 30-year period as part of an amyloidosis referral practice. PubMed was searched through January 2025 for the terms: amyloidosis, amyloid, Sjogren’s syndrome, and their combinations.
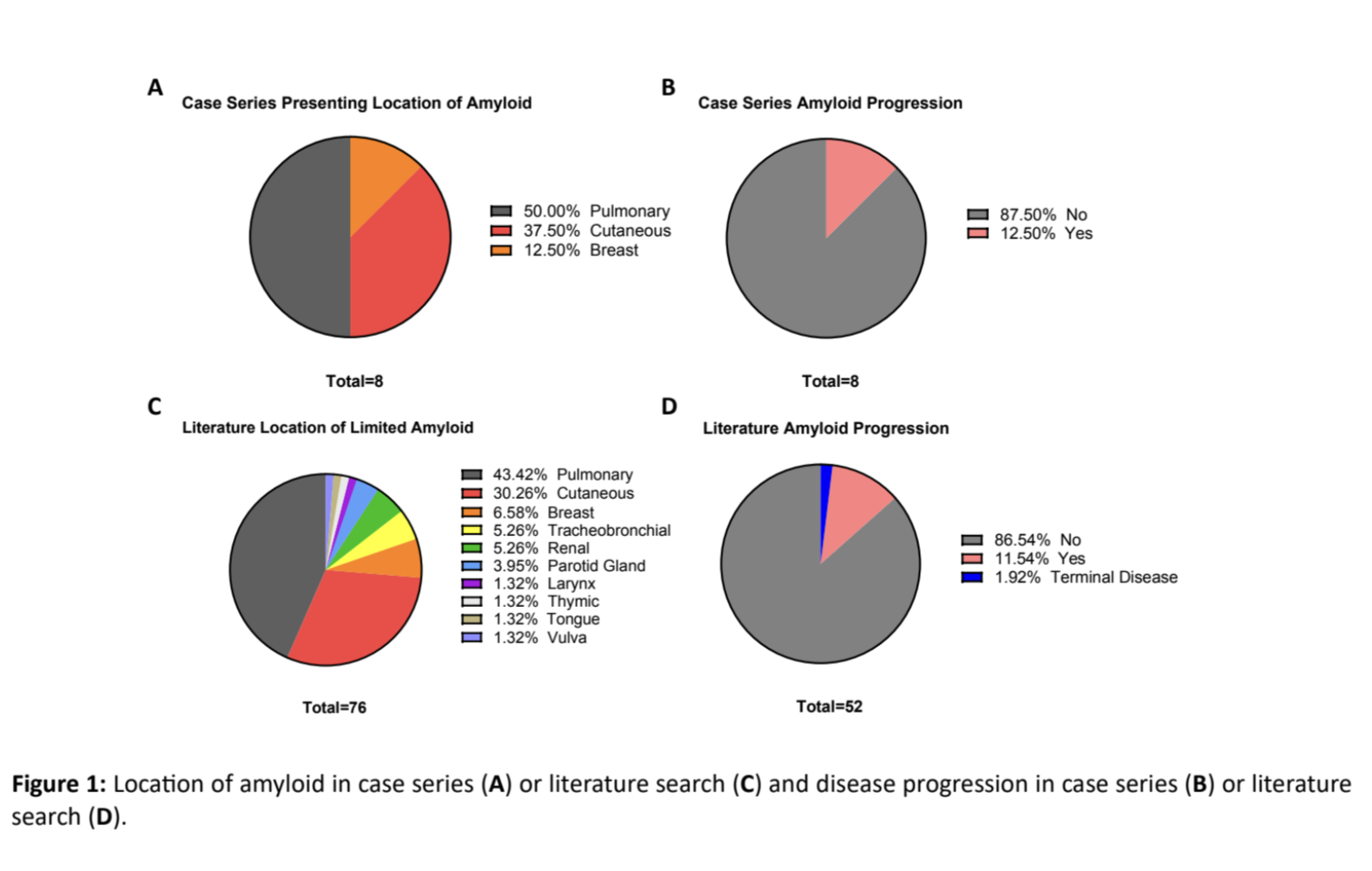
Results: -In our cohort, the average age of SS at diagnosis was 40.9 (range 17-54). The average age at the time of amyloidosis diagnosis was 51.6 (range 37-73). 7/8 patients developed amyloid after being diagnosed with KCS/SS 12.3 years prior (range 5-22). In the remaining patient, SS and amyloidosis were diagnosed concurrently. The diagnosis of amyloidosis was made by immunohistochemistry and amyloid typing by sequence analysis, including mass spectrometry (7/8 patients). All samples stained positive for Congo red, and 8/8 were the AL subtype. Six patients had AL (λ), one had AL (κ), and in one patient both light chain types were present. All eight patients initially presented with localized amyloidosis, with no indication of systemic disease on detailed work-up. Of these patients, 4 had pulmonary amyloidosis, 3 had cutaneous amyloidosis, and 1 had intraparenchymal breast amyloidosis (Figure 1A). During the averaged 8.6 year follow-up (range 1-21), only the patient with intraparenchymal breast amyloid progressed to have systemic disease. In this patient, a pulmonary amyloid lesion presented six years after the original amyloid diagnosis. The remaining seven patients have had stable disease (Figure 1B; Table 1). -We performed a literature search for articles published on SS and amyloidosis and found 55 publications comprising 74 total patients. The mean age of diagnosis of SS was 52, while amyloidosis was diagnosed at 59. The predominant subtype was AL (κ) (39.7%), followed by AL (λ) (19.05%). Most patients presented with local amyloidosis (92.68%) with the most common location being pulmonary (43.42%), cutaneous (30.26%), and breast (6.58%) (Figure 1C). Of those reported, 86.54% with localized disease did not have disease progression, 11.54% did have progression, and one patient had terminal disease (Figure 1D).
Conclusion: -In our long-term follow-up of amyloidosis in SS, we monitored for local and systemic progression for an average duration 8.6 years (range 1-21 years).-Between our cohort and our literature search, we find the most common location for amyloidosis in SS is pulmonary, then cutaneous, and finally breast.-While the majority of cases are stable and do not progress, a subset of patients do, requiring close monitoring.
.jpg) Case series progression follow-up
Case series progression follow-up
.jpg) Location of localized amyloid and disease progression in case series versus literature review.
Location of localized amyloid and disease progression in case series versus literature review.
To cite this abstract in AMA style:
Nguyen H, Moresco P, Chiu A, Patnaik A, Gorevic P. Characterization and Progression of Localized Amyloidosis in Sjogren’s Syndrome: Evidence Long-Term (1995-2025) Follow-Up of a Cohort compared to Literature Review. [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/characterization-and-progression-of-localized-amyloidosis-in-sjogrens-syndrome-evidence-long-term-1995-2025-follow-up-of-a-cohort-compared-to-literature-review/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/characterization-and-progression-of-localized-amyloidosis-in-sjogrens-syndrome-evidence-long-term-1995-2025-follow-up-of-a-cohort-compared-to-literature-review/