Session Information
Session Type: Poster Session B
Session Time: 9:00AM-10:30AM
Background/Purpose: Patients with JIA are at an increased risk of loss to follow-up, morbidity and mortality as they transition from pediatric to adult care. Thus, adult rheumatologists must understand the disease-related characteristics of their incoming JIA patients to provide appropriate care and support. Initiated in 2017, the Canadian Alliance of Pediatric Rheumatology Investigators (CAPRI) JIA registry prospectively collects disease-related outcomes among newly (< 3 months) diagnosed JIA patients. We aimed to characterize disease activity and disease-related outcomes of adolescents with JIA, prior to their transfer to adult care.
Methods: We obtained data from patients in the CAPRI registry whose 17-year-old data collection was complete by December 2021. These include newly diagnosed patients with JIA and data from established patients from two additional Canadian JIA cohorts (Linking Exercise, Activity and Pathophysiology in Childhood Arthritis [LEAP] and Research in Arthritis in Canadian Children emphasizing Outcomes [ReACCh-Out]). At each clinic visit, the most responsible physician (MRP) completed a questionnaire on disease activity, treatment and adverse events. The MRP completed an additional questionnaire once the patient reached age 17 to characterize disease-related damage. Patient-reported outcomes (as measure on a 21-point Likert scale, 0-10) included pain scores, patient global assessment of disease activity and Quality of My Life. Descriptive statistics were used to characterize patients’ disease activity, disease-related outcomes and medication use at age 17 and changes that occurred in the year prior to transfer to adult care.
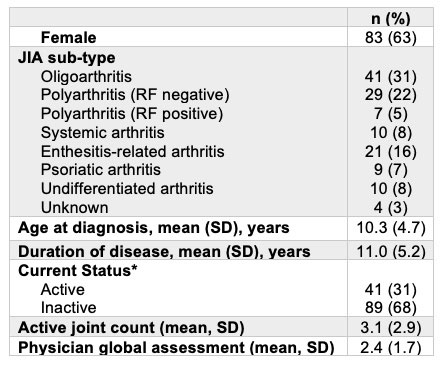
Results: One hundred and thirty-one 17-year-olds (63% female, mean (SD) age at diagnosis 10.3 (4.7) years), were included (Table 1). Most patients (n=129) were taking medications prior to transfer, including NSAIDs (n=45), methotrexate (n=45), biologic agents (n=44), oral (n=5) or ocular steroids (n=1). Mean (SD) scores for patient pain, patient global assessment of disease activity, and Quality of My Life scores were 3.7 (2.7), 3.3 (2.8), and 7.7 (2.6), respectively. Changes in disease course one year prior to transition are shown in Table 2. Among 80 (59.7%) patients whose data were available for the 17-year-old questionnaire, half (n=41, 51.3%) were in remission (Table 3). Clinically detectable joint damage was present in 21 (26%) patients, while 25 (31%) had radiographic damage. The TMJ, wrists and hips were most commonly affected. Few patients were ever hospitalized (n=6) or experienced serious adverse events (n=5).
Conclusion: Among this Canadian cohort of JIA patients, one third had active disease and almost all were taking medications prior to transfer to adult care. One third had radiographic joint damage while one quarter had clinically detectable joint damage, with the TMJ being the most commonly affected joint. Patient reported outcomes were generally favourable. This study highlights the disease burden transitioning patients carry at the vulnerable time of transfer to adult care. These results will help adult rheumatologists anticipate the medical needs of newly transitioned patients given the degree of active disease and extent of medication use.
To cite this abstract in AMA style:
Semalulu T, BEATTIE K, Berard R, Guzman J, Batthish M. Characteristics of Transitioning JIA Patients: Who Is Arriving on the Adult Rheumatologists’ Doorsteps? [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/characteristics-of-transitioning-jia-patients-who-is-arriving-on-the-adult-rheumatologists-doorsteps/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/characteristics-of-transitioning-jia-patients-who-is-arriving-on-the-adult-rheumatologists-doorsteps/