Session Information
Date: Monday, November 13, 2023
Title: (1200–1220) Patient Outcomes, Preferences, & Attitudes Poster II
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Rheumatic diseases such as rheumatoid arthritis (RA) and Systemic lupus erythematosus (SLE) were known for increased prevalence and risk of death from cardiovascular disease (CVD) due to systemic inflammation in conjunction with other environmental risk factors and genetic predispositions. 1 The COVID-19 pandemic is of the leading causes for the increased age-adjusted mortality rate in 2020 due to various unforeseeable conditions including unequitable healthcare resource distribution, decrease access to medical treatment other than for COVID-19 infection. 2
To investigate if the presence of the COVID-19 had an impact on the mortality outcome of acute myocardial infraction (AMI) and acute heart failure (AHF) in rheumatic diseases (RDs) including patients with RA, SLE, scleroderma, psoriasis/psoriatic arthritis, gout, myositis and vasculitis, and sarcoidosis in the United States using the NIS inpatient database from 2016-2020.
Methods: Using NIS database from 2016-2020, which stratifies 20% of the total national hospital admissions, we identified patients with a primary admission diagnosis (s) of AMI or AHF (with concurrent COVID-19 infection for 2020 data) using ICD-10 codes. (Table.1) For each admission, we calculated the baseline characteristics including mortality risk with independent variable for present or absence of RDs’ ICD10 codes as the secondary diagnosis. The association of RDs with inpatient mortality was calculated using multivariable logistic regression.
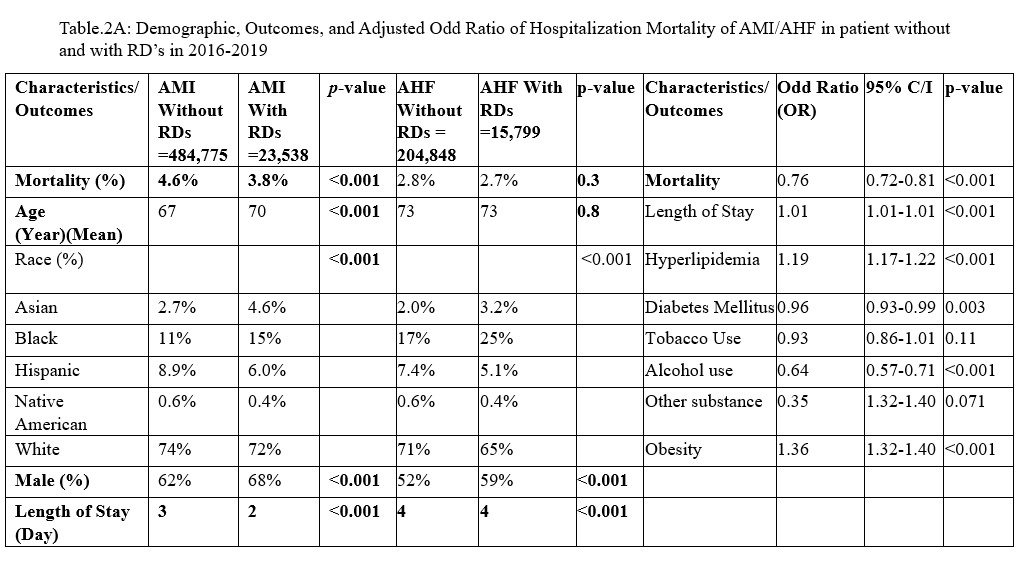
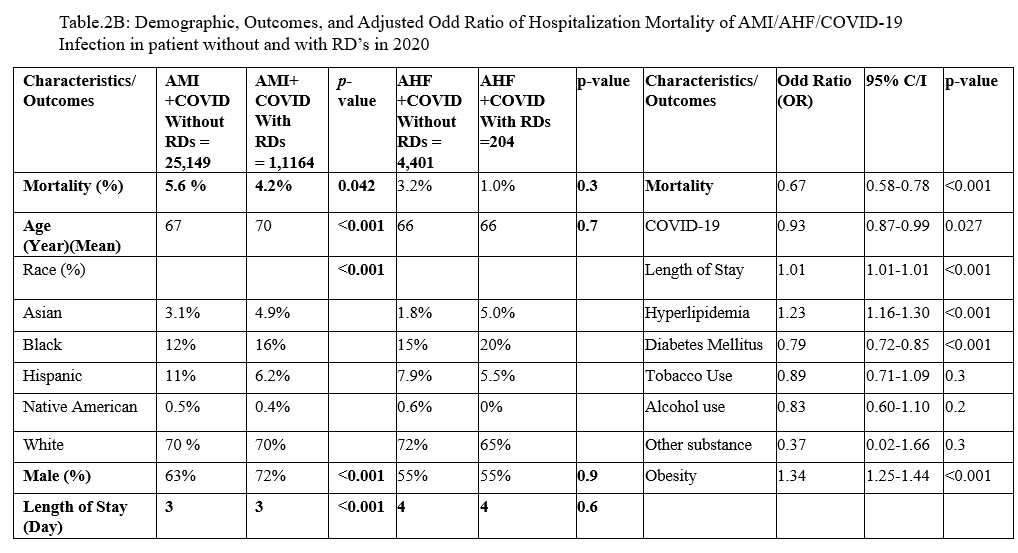
Results: For 2016-2019, there were 484,775 AMI admissions without underlying RDs comparing to 23,538 AMI with RDs. During this pre-COVID-19 pandemic time, the inpatient mortality was significantly higher in the non-RDs (4.6% vs. 3.8%, p< 0.001). For AHF hospitalizations, 204,848 admissions were non-RDs compared to 15,799 RDs. There was no significance in term of mortality between these two groups. (2.8% vs. 2.7%, p=0.3) The odd of dying from AMI and AHF in patients with RDs was less compared to patients in the non-RDs group after adjusting for age, race, gender, regions and other confounders. (OR=0.76, p< 0.001) (Table.2A) For the pandemic year, there were 26,313 total AMI/COVID-19 infection hospitalizations, whereas 1,164 of these admissions were from patients with RDs. The mortality was still more significant in the non-RDs group. (5.6% vs. 4.2%, p=0.042) For the AHF/COVID-19 infection hospitalization, total of 4,405 with 204 of them were from the non RDs group. Due to smaller sample size, the mortality was not significant higher in the non-RDs group. (3.2% vs. 1.0%, p=0.073) In terms of the combined mortality OR of AMI/AHF/COVID-19 infection for 2020, the non-RDs group was still having lower odd compared to RDs group (Table.2B).
Conclusion: Based on our analysis, the presence of co-morbid RDs was not associated with increase mortality in patients hospitalized with AMI even with coexisting COVID-19 infection. For the AHF cohort, there was no significance in mortality in both groups. A detailed cardiovascular review of systemic during each rheumatology clinic visit may have helped to implement early intervention on CVD complications in RDs by early referral to cardiology.
To cite this abstract in AMA style:
Li Z, Huang S, Gokcebel s, Reginato A. Cardiovascular Mortality of Acute Myocardial Infraction and Acute Heart Failure Hospitalization in Rheumatic Diseases Patients Evaluation from the 2016-2020 National Inpatient Sample (NIS) Database [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/cardiovascular-mortality-of-acute-myocardial-infraction-and-acute-heart-failure-hospitalization-in-rheumatic-diseases-patients-evaluation-from-the-2016-2020-national-inpatient-sample-nis-database/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/cardiovascular-mortality-of-acute-myocardial-infraction-and-acute-heart-failure-hospitalization-in-rheumatic-diseases-patients-evaluation-from-the-2016-2020-national-inpatient-sample-nis-database/