Session Information
Date: Monday, November 8, 2021
Session Type: Poster Session C
Session Time: 8:30AM-10:30AM
Background/Purpose: Inflammatory arthritis (IA) is associated with cardiovascular disease (CVD). Cardiac biomarkers may assist with CVD risk stratification. We aimed to estimate the prevalence, and correlates of abnormal cardiac biomarkers in IA.
Methods: A cross-sectional study of consecutive patients enrolled in the University of Toronto Cardio-Rheumatology Network from 2017 to 2020 was performed. This is a primary CVD prevention program with structured clinical and laboratory assessments to diagnose and treat CVD. Patients are eligible if they have rheumatoid arthritis (RA) or spondyloarthropathy (SpA, psoriatic arthritis or ankylosing spondylitis), and no documented CVD. We included patients with baseline data for 5 cardiac biomarkers and examined the prevalence of abnormal biomarkers according to site-specific lab cut-offs: high-sensitivity troponin T (hs-TnT) (≥15 ng/L), N-terminal prohormone BNP (NT-proBNP, ≥35 pmol/L or 100 pg/mL), Apolipoprotein A1 (ApoA1, ≤1.96 g/L), Apolipoprotein B (ApoB, ≥1.17g/L or ≥1.46g/L ) and Lipoprotein a (Lp(a) ≥9.7mg/dL or ≥30mg/dL). We performed logistic regression to evaluate the association with IA diagnosis and each biomarker, adjusted for demographic, clinical and CVD risk factors.
Results: A total of 376 participants were included. The majority had RA (58%), followed by PsA (33%) and AS (9%). Mean (SD) age of the sample was 59 (10.5) years and 70% were female. Disease activity and acute phase reactants reflected well controlled disease and treatment consisted primarily of csDMARDs (63%) or bioDMARDs (39%) (Table 1). At least 1 CVD risk factor was present in 77% of subjects, most commonly current/ever smoking (47%), obesity (35%), hypertension (33%) or dyslipidemia (27%). Thirteen percent had elevated hs-TnT and 17% had elevated NT-proBNP (Table 2). Abnormal lipid biomarkers occurred in 45%, primarily due to abnormal Apo A1 (90%) and to a lesser degree abnormal Lp (a) levels (29%, Table 2). Subjects with RA were more likely to have abnormalities in NT-proBNP and ApoB, but had more favourable HDL-c, non-HDL-c and triglyceride profiles compared to the PsA/AS group (Table 2). In multivariate analyses, increasing age was significantly associated with abnormal hs-TnT and NT-proBNP but negatively associated with ApoB. Female sex was associated with greater odds for abnormal Lp (a) but lower values of hs-TnT and NT-proBNP (Table 3). No other IA disease-specific or CVD risk factors were consistently associated with cardiac biomarkers (Table 3).
Conclusion: Abnormalities in cardiac and lipid biomarkers are common even in well-controlled IA patients with no known CVD. Additional research is needed to determine if biomarkers may help with CVD risk re-classification beyond traditional clinical risk score approaches. In addition, it will be important to understand whether CVD biomarkers are responsive to changes in disease activity or particular therapies, which may be another rationale for a treat-to-target approach in IA.
 Table 1. Baseline characteristics by inflammatory arthritis diagnosis.
Table 1. Baseline characteristics by inflammatory arthritis diagnosis.
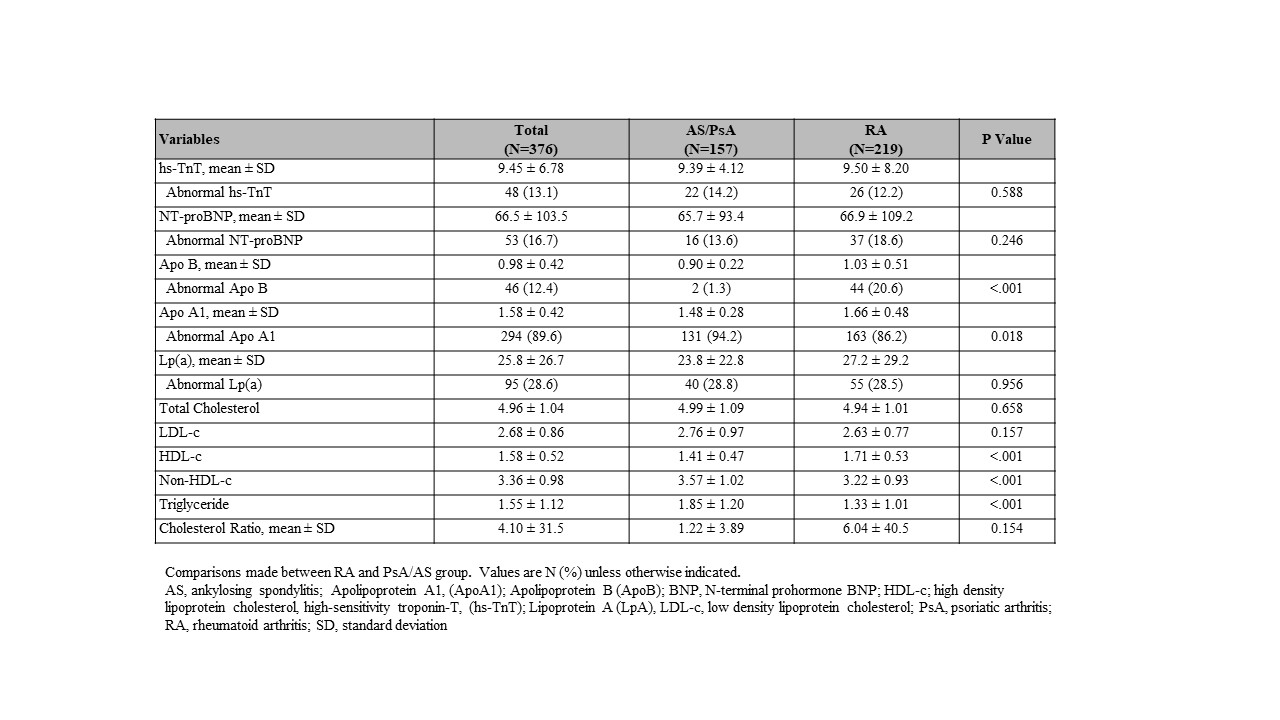 Table 2. Prevalence of cardiac biomarkers by inflammatory arthritis diagnosis.
Table 2. Prevalence of cardiac biomarkers by inflammatory arthritis diagnosis.
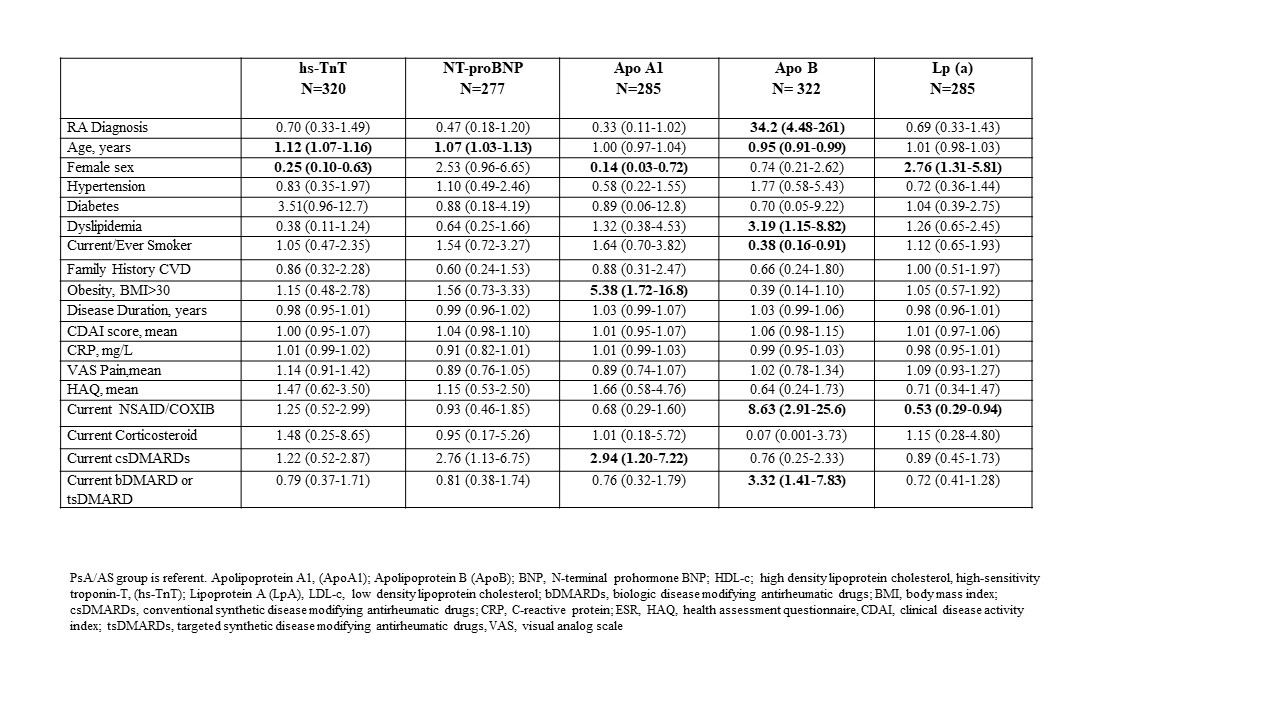 Table 3. Multivariate logistic regression analysis of baseline characteristics for abnormal cardiac biomarkers.
Table 3. Multivariate logistic regression analysis of baseline characteristics for abnormal cardiac biomarkers.
To cite this abstract in AMA style:
Kuriya B, Akhtari S, Movahedi M, Udell J, Lawler P, Harvey P, Eder L. Cardiovascular and Lipid Biomarker Distributions in Inflammatory Arthritis [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/cardiovascular-and-lipid-biomarker-distributions-in-inflammatory-arthritis/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/cardiovascular-and-lipid-biomarker-distributions-in-inflammatory-arthritis/
