Session Information
Session Type: Poster Session (Sunday)
Session Time: 9:00AM-11:00AM
Background/Purpose: The association of vitamin D deficiency with SLE is well established. While disease activity can itself cause pathologic bone remodeling and reduced vitamin D, SLE flares often necessitate steroid treatment, which can lead to decreased vitamin D absorption and decreased bone mineral density. Some rheumatologists recommend a goal serum 25(OH)D of 40ng/mL to reduce the probability ratio for a high disease activity score and to also improve urine protein-to-creatinine ratio. In addition, the ACR recommends vitamin D replacement for all patients receiving steroids, irrespective of steroid dose or duration of treatment.
The objective of this study is to identify practice care gaps among rheumatologists in their adherence to vitamin D replacement in SLE patients currently on steroid therapy. An additional practice review of evaluating for vitamin D deficiency is noted.
Methods: Data collected from the Southern California Lupus Registry (SCOLR), an academic cohort of 182 patients with SLE, was analyzed. Cross-sectional review of medical records of patients seen from June 2016 to April 2019 included the following data: 1) Current or prior use of systemic steroids, 2) Vitamin D replacement in patients receiving steroid therapy, 3) Evaluation of vitamin D level within 6 months of patient encounter. Independent review was completed on medications prescribed. Abnormal vitamin D level was deemed < 30ng/mL. Descriptive statistics were utilized. This study is approved by the Loma Linda University IRB.
Results: Of 182 patients enrolled in SCOLR, data was available to be analyzed in 176 (Figure 1). Current, prior and never use of steroids was noted in 56 (32%), 73 (41%), 47 (27%), respectively. In patients currently on steroids, vitamin D replacement was provided to 30 (54%).
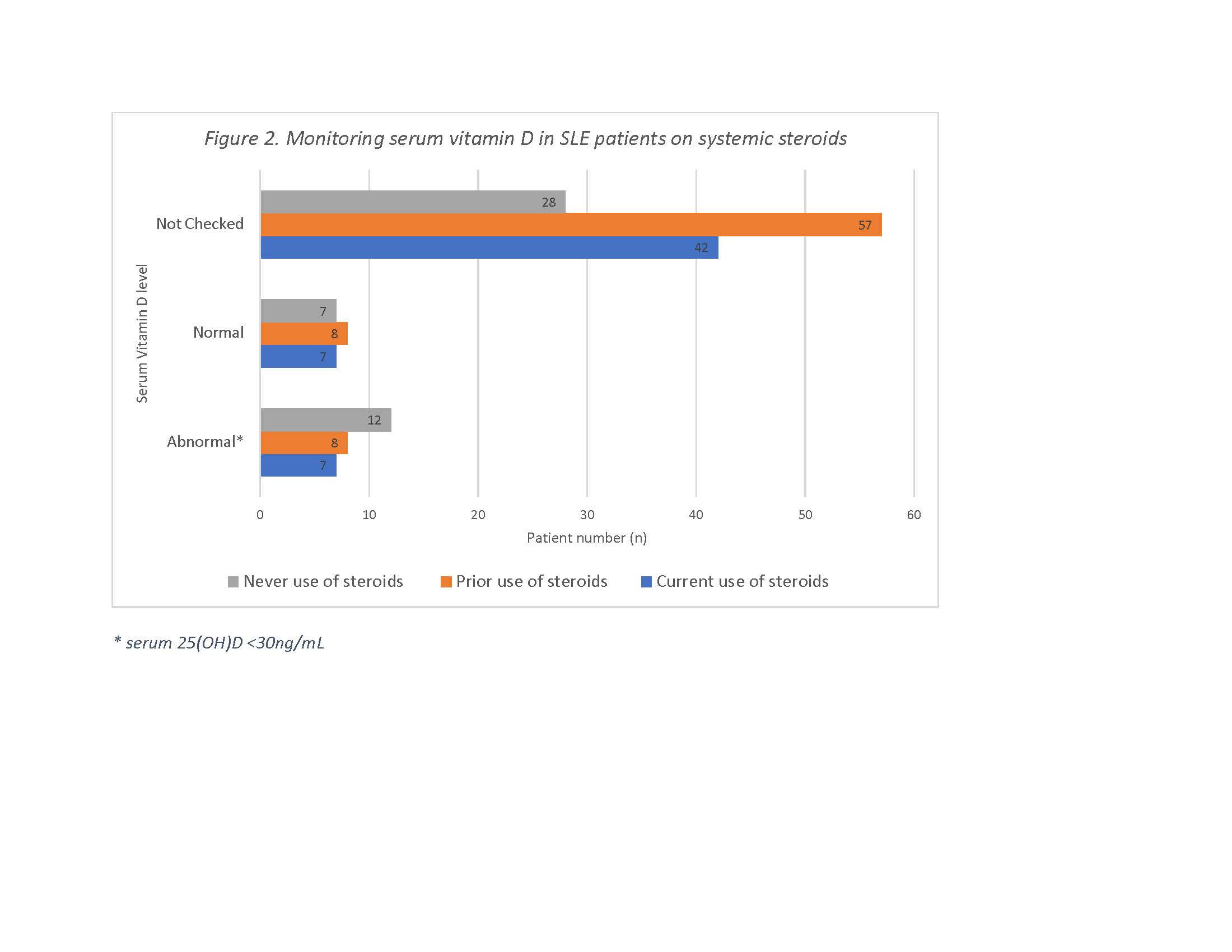
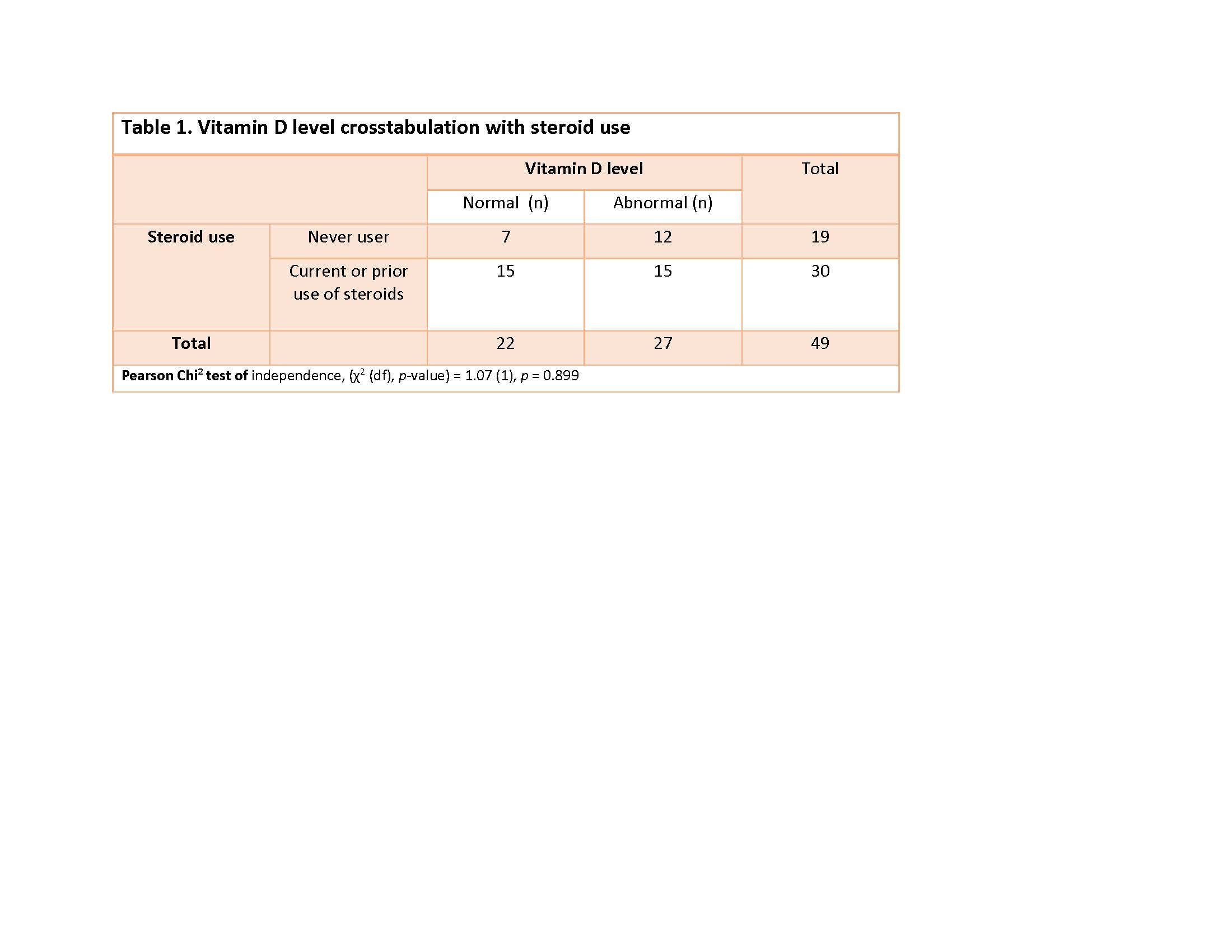
Vitamin D levels were tested in 49/176 (28%) and noted to be abnormal in 27/49 (55%) (Table 1). Contrary to our expectations, patients with current or prior use of systemic steroids did not experience a significantly increased risk of abnormal vitamin D levels (OR 0.583, 95% CI (0.18, 1.89). However, vitamin D level was not checked in 42/56 (24%) patients currently on steroids and 57/73 (78%) patients with prior use of steroids, which limits the ability to formulate more meaningful conclusions.
Conclusion: Rheumatologists are infrequently screening for vitamin D deficiency in SLE. Further, vitamin D supplementation is inadequate in those individuals receiving systemic steroids. We acknowledge our gaps in the power of this study but bring to light the need for increased awareness of bone health in SLE in addition to the appropriate management of such individuals exposed to systemic steroids. With this information, we will plan to implement a best practice advisory warning in the electronic medical record of all individuals receiving steroid therapy to trigger both screening for and treating vitamin D abnormalities. Additional attention is warranted in monitoring and replacing vitamin D a complementary treatment of SLE, which will be the studied further as a continuation of this analysis.
To cite this abstract in AMA style:
Sandhu, MBBS V, Johnson S. Bone Health in Lupus: Findings from the Southern California Lupus Registry [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/bone-health-in-lupus-findings-from-the-southern-california-lupus-registry/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/bone-health-in-lupus-findings-from-the-southern-california-lupus-registry/