Session Information
Session Type: Poster Session B
Session Time: 9:00AM-10:30AM
Background/Purpose: Disc space narrowing (DSN) at the intervertebral disc and vertebral osteophyte (OST) formation are two potential sources of nociceptive lower back pain (LBP). The most significant biological reason for DSN is a loss of proteoglycans found in the extracellular matrix of the nucleus and annulus. As such, biomarkers that reflect proteoglycan content may improve our understanding of the etiological changes that occur during a degenerative process. Inflammation may also accelerate DSN and OST formation. In addition, pressure-pain threshold (PPT), a marker of pain sensitivity, has been found to predict LBP. Therefore, the objective of this study is to determine if baseline biomarkers or PPT predict the worsening of DSN, OST, or LBP in a community-based sample.
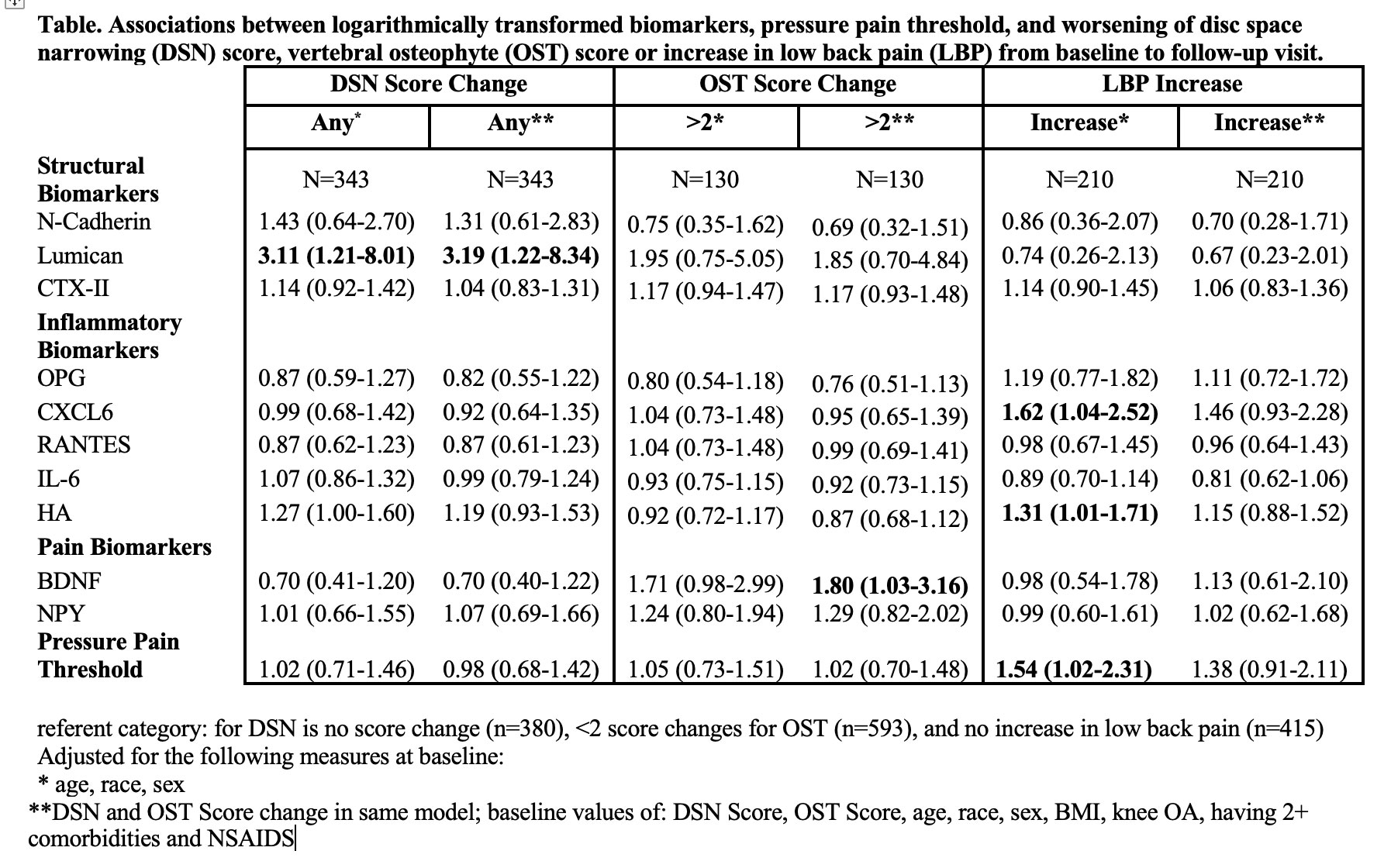
Methods: Paired baseline (2003-2004) and follow-up (2006-2010) lumbar spine radiographs from the Johnston County Osteoarthritis Project were graded for severity (0-3) of DSN and OST. Severity scores were summed across the five lumbar spine levels to create separate total DSN and OST scores. LBP severity (none, mild, moderate, or severe) was self-reported. LBP was considered worsening if there was a ≥ 1-categorical increase in severity from baseline to follow-up. Concentrations of N-cadherin, Keratin-19, Lumican, CXCL6, RANTES, HA, CTX-II, IL-6, BDNF, OPG, and NPY analytes were quantified by immunoassay. A standard dolorimeter measured PPT. Multiple binary logistic regression models were used to estimate odd ratios (OR) and 95% confidence intervals (CI) of PPT (pain threshold at < 4KG or ≥4kg) or logarithmically transformed biomarker levels predicting worsening of DSN, OST or LBP. Initial models were adjusted for age, sex and race; separate models were further adjusted for body mass index (BMI), self-reported NSAID use and comorbidities, radiographic knee OA defined as Kellgren-Lawrence grade < =2 versus >2, baseline values of DSN or OST, and score change of DSN or OST as appropriate.
Results: The sample consisted of 731 participants with available data. Over 2/3 were women, 1/3 were African American, the average age was 66.1 years and average BMI was 31.4 kg/m2. Over 1/3 had knee OA, 1/3 had > two comorbidities, and nearly 2/3 reported NSAID use. The Table describes the results for biomarkers, pressure-pain threshold and DSN, OST and LBP. Lumican, reflecting changes to the proteoglycan content within the extracellular matrix, was a consistent and strong predictor of DSN worsening (OR=3.19 95% CI 1.22, 8.01). BDNF (OR=1.80 95% CI 1.03, 3.16) was a predictor of OST worsening, which may reflect osteoclastogenesis. HA and CXCL6, indicative of systemic inflammation, and perceived pressure pain sensitivity measured by PPT were significant predictors of increased LBP severity: OR=1.31 (95% CI 1.01, 1.71), OR=1.62 (95% CI 1.04, 2.52), and OR=1.54 (95% CI 1.02, 2.31), respectively. After adjustment for covariates, these relationships were no longer statistically significant.
Conclusion: Our findings suggest utility of biomarkers and PPT for predicting worsening of lumbar spine structure degeneration and LBP. Biomarkers differed by anatomical composition between DSN and OST suggesting specificity for lumbar spine structure.
To cite this abstract in AMA style:
Goode A, Cleveland R, Kraus V, George S, Taylor K, Schwartz T, Renner J, Huebner J, Golightly Y. Biomarkers Predict Worsening of Lumbar Spine Degeneration and Low Back Pain: The Johnston County Osteoarthritis Project [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/biomarkers-predict-worsening-of-lumbar-spine-degeneration-and-low-back-pain-the-johnston-county-osteoarthritis-project/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/biomarkers-predict-worsening-of-lumbar-spine-degeneration-and-low-back-pain-the-johnston-county-osteoarthritis-project/