Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Renal involvement in primary APS is underrecognized and histologically diverse, encompassing both vascular and glomerular pathology. We aimed to describe the histopathology, outcomes of biopsy-proven renal disease among primary APS and predictors of renal involvement.
Methods: Among 233 patients with primary APS (revised Sapporo criteria, 2006), Renal abnormalities defined as proteinuria >0.5 g/day and/or elevated serum creatinine with or without hematuria—were identified. Clinical, serological, histopathological and direct immunofluorescence (DIF) data were analyzed. Renal lesions were classified as per the Renal Pathology Society-2023 consensus definitions for aPL- nephropathy.
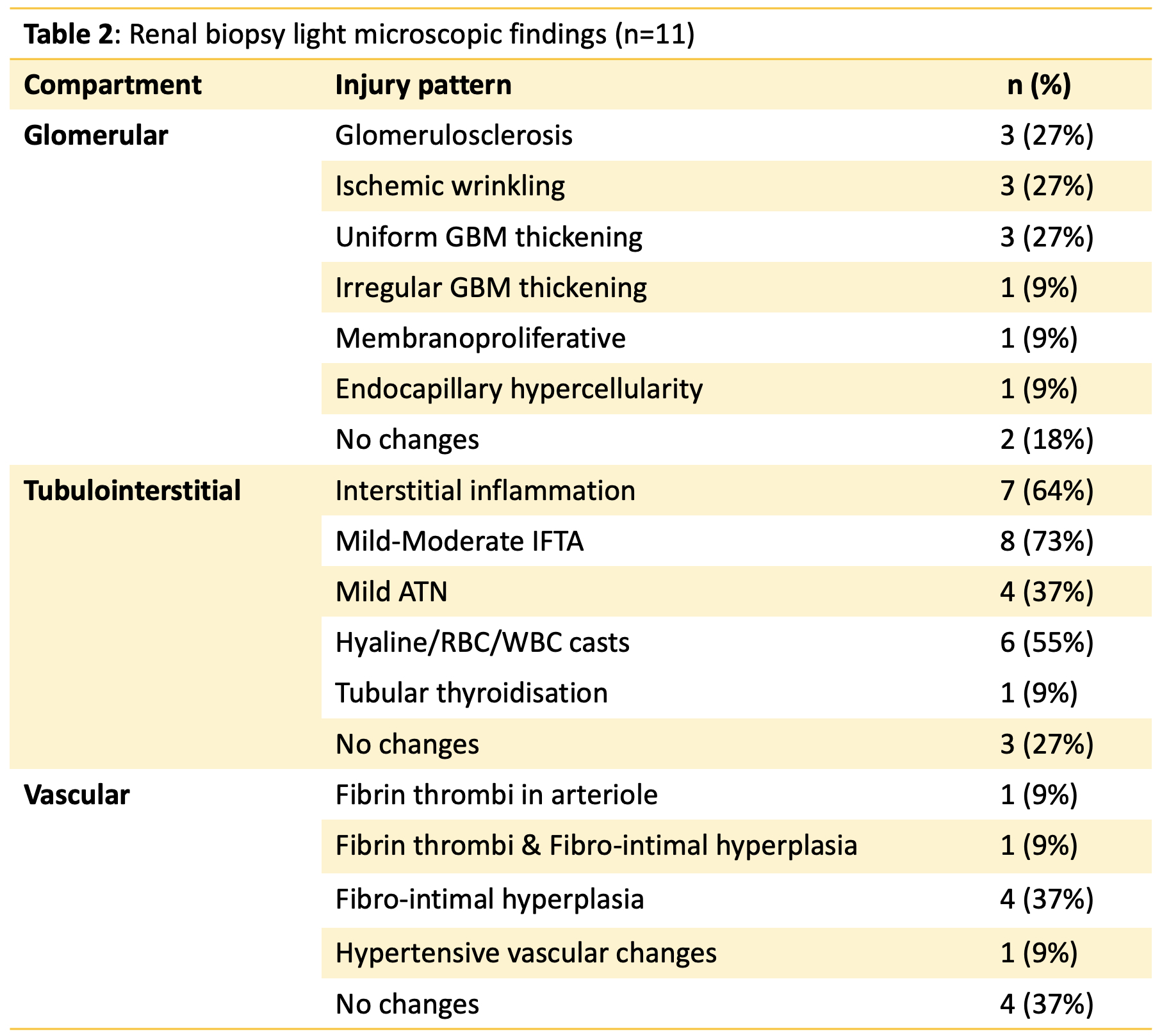
Results: Nineteen patients (8.15%) had renal abnormalities, Of these, 11 patients underwent kidney biopsy (Table 1). The median age of the biopsied cohort was 27 years (23.5-38), with 63.6% female. Hypertension was present in 63.6%. Median serum creatinine was 1.6 mg/dL (0.75-2.35), and UPCR was 4.4 g/g (1.76-7.5).Renal biopsy findings were diverse (Figure 1A), with glomerular injury more frequent than aPL nephropathy. The major glomerular finding was glomerulosclerosis and ischemic wrinkling of GBM (a sequela of TMA) seen in 27%, followed by basement membrane thickening, while interstitial inflammation was present in 64% and mesangial expansion in 73% (Table 2). Isolated Antiphospholipid nephropathy (aPL-N) was seen in 2/11 patients. Acute or chronic TMA like lesions with immune deposits or inflammatory cells seen in 4/11 patients (54.5%). Acute TMA lesions were seen in one patient, chronic lesions seen in four, while one patient had acute with chronic TMA change (Table 2). DIF was positive in most, with a full-house pattern observed in two patients, despite no lupus manifestations (Figure 1B).Treatment included warfarin (n=9, 81.8%), RAAS blockade (n=10, 90.9%), corticosteroids (n=4, 36.4%), and MMF (n=3, 27.3%). In the biopsied group (n=11), at a median 2-year follow-up, four (36.4%) achieved complete proteinuria remission (UPCR < 0.5 g/g), two (18.2%) had partial reduction, and one (9%) patient showed resolution of AKI. Of all 19 APS with renal manifestations, five had CKD and only one progressed to dialysis-dependent ESRD.On univariate analysis, arterial thrombosis (p = 0.002) and cutaneous ulcers (p = 0.0009) were significantly associated with renal involvement. On multivariable logistic regression, cutaneous ulcers independently predicted renal involvement (OR:19.5, 95% CI: 1.37-277.8, p=0.028), suggesting microvascular skin–renal overlap.
Conclusion: Renal abnormalities were identified in 8.2% of patients with primary APS. Only a minority of biopsied patients met strict histological criteria for aPL nephropathy. Most biopsies showed glomerular immune deposits or interstitial inflammation, pointing to immune-mediated renal injury in APS patients. The histologic overlap with SLE supports a pathologic continuum. Given the multitude of renal biopsy findings in Primary APS, it calls for individualized, pathology-driven treatment. Renal outcomes were favorable, with a low incidence of dialysis-requiring CKD.
 Renal Involvement in Primary APS: Clinical Characteristics, Biopsy Findings, and Outcomes in 11 Patients
Renal Involvement in Primary APS: Clinical Characteristics, Biopsy Findings, and Outcomes in 11 Patients
To cite this abstract in AMA style:
MISHRA R, PHILIP S, NAUSHAD R, GOPAL A, Kavadichanda C, MARIASELVAM C, N G R, Thabah M, NEGI V. Beyond Thrombosis: Histological Spectrum, Predictors and Outcomes of Renal Involvement in Primary Antiphospholipid Syndrome: A Single-Centre Cohort Study [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/beyond-thrombosis-histological-spectrum-predictors-and-outcomes-of-renal-involvement-in-primary-antiphospholipid-syndrome-a-single-centre-cohort-study/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/beyond-thrombosis-histological-spectrum-predictors-and-outcomes-of-renal-involvement-in-primary-antiphospholipid-syndrome-a-single-centre-cohort-study/

.jpg)
.jpg)