Session Information
Date: Monday, October 27, 2025
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Sjogren’s disease (SjD) is a systemic autoimmune disorder characterized by inflammatory involvement of the exocrine glands and extra-glandular manifestations. Among the latter, there is a growing interest in the study of neurological involvement, as the prevalence and association factors are still divergent in the literature. Thus, the objective was to evaluate the frequency of neurological manifestations in SjD, as well as the laboratory factors associated with the disease.
Methods: This retrospective observational study reviewed the electronic medical records of patients diagnosed with SjD, according to the 2002 or 2016 ACR criteria, at a tertiary outpatient clinic. Only patients over 18 years of age with the primary form of the disease were included. Patients with neurological manifestations were assessed and reviewed to determine whether the manifestations could be attributed to SjD. When attributable, their types and frequencies in the study population and their association factors were described. Inferential analysis was performed by comparing patients with neurological manifestations and those without neurological manifestations with regard to the presence of anti-Ro, anti-La, ANA, rheumatoid factor, C3, C4, cryoglobulins, hypergammaglobulinemia or hypogammaglobulinemia using Fischer and Chi Square statistical methods and, if necessary, multivariate analysis with logistic regression.
Results: 92 patients with SjD were evaluated. A prevalence of 17,39% neurological manifestations was found in the context of SjD in the peripheral nervous system (PNS). The main types of PNS found were ganglionopathy, sensitive neuropathy, multiple mononeuritis, fine fiber neuropathy and sensitive-motor neuropathy and are illustrated in figure 1. The two patients with CNS manifestations were attributed to concomitant Neuromyelitis Optica Spectrum Disease. Thus, a comparative inferential analysis was carried out between laboratory markers and the presence of PNS manifestations. In the univariate analysis, only hypogammaglobulinemia showed a significant statical association (p = 0.008). This association also occurred in the multivariate analysis, using rituximab as a covariate (p = 0,010). Table 1 shows the results obtained after statistical analysis.
Conclusion: In our sample, we found a prevalence of approximately 17,39% of neurological manifestations, with only PNS involvement attributable to SjD. The two CNS manifestations found to be immune in nature were attributed to the Neuromyelitis Optica spectrum disorder. Hypogammaglobulinemia, independent of rituximab use, was the only variable associated with PNS manifestations.
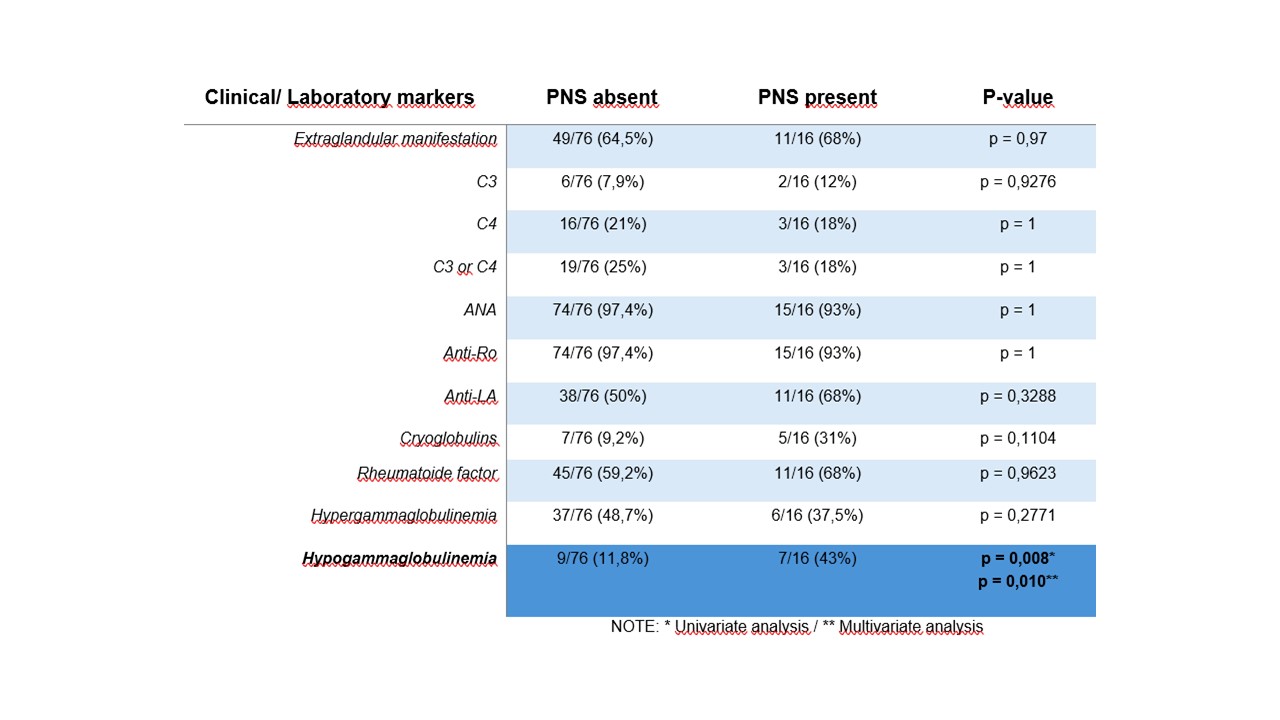 Figure 1: Types of neurological manifestations of PNS attributable to Sjögren’s disease
Figure 1: Types of neurological manifestations of PNS attributable to Sjögren’s disease
.jpg) Table 1: Statistical analysis comparing patients with Sjögren’s Disease with and without associated peripheral neuropathy
Table 1: Statistical analysis comparing patients with Sjögren’s Disease with and without associated peripheral neuropathy
To cite this abstract in AMA style:
Fróes Ramos de Lima R, Sewa Marques R, Sachetto Z, Pugliesi A. Beyond the Glands: Hypogammaglobulinemia as a Clue to Peripheral Neuropathy in Sjogren´s Disease [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/beyond-the-glands-hypogammaglobulinemia-as-a-clue-to-peripheral-neuropathy-in-sjogrens-disease/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/beyond-the-glands-hypogammaglobulinemia-as-a-clue-to-peripheral-neuropathy-in-sjogrens-disease/
