Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Bronchiectasis (BC) has been observed in association with Systemic Sclerosis (SSc). Esophageal dysmotility, immunosuppressive drugs and the direct effect of collagen deposition in the airway are postulated as causes of bronchiectasis in patients with SSc. We aim to evaluated the bronchiectasis prevalence in an SSc population and its possible association with clinical and immunological features.
Methods: Observational, analytical and cross-sectional monocenter study. We included 92 patients with diagnosis of SSc according to modified ACR-EULAR 2013 criteria, who had undergone high-resolution computed tomography (HRCT) of the chest within the last two years. Patients with traction bronchiectasis associated to pulmonary fibrosis were excluded. Continuous variables were compared by Student’s or Mann Whitney’s T test, and categorical variables by Chi2 test or Fisher’s exact test.
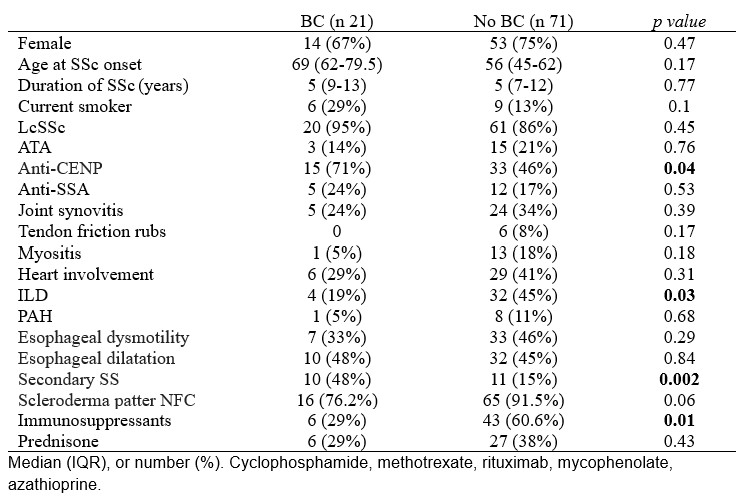
Results: In 21 (23%) of the patients, bronchiectasis were present (within fibrosis or honeycomb). Median age was 61 (52-67.5), 67% were female and 48% had a smoking history. No patient has a previous personal history of Mycobacterium tuberculosis infection. Two patients suffer from chronic cough but neither presented with pulmonary infectious complications. No significant association between bronchiectasis and esophageal dysmotility or dilatation (observed in 33% and 46% respectively), any demographic variable, SSc duration or cutaneous subclass (Table 1). Patients with bronchiectasis were more likely to be Anti-CENP positivity (p=0.044) and had a higher rate of secondary Sjogren’s syndrome (p=0.006). There were no differences in pulmonary function tests between patients without ILD and patients with bronchiectasis (DLCO 76% vs 72%, FVE1/FVC1 82% vs. 80%). Interstitial lung disease and immunosuppressants had a negative association with bronchiectasis (p=0.032 and p=0.01).
Conclusion: Bronchiectasis should be included in the list of pulmonary manifestations of SSc, a negative association between bronchiectasis and ILD reflects that bronchiectasis is an independent entity. Given that bronchiectasis was more frequent in patients with secondary Sjogren’s syndrome, but not in SSA-positive participants, we hypothesize that its development is related to sicca symptoms in the tracheobronchial tree. Since neither esophageal nor immunosuppressive involvement was found as a cause of bronchiectasis, the infectious origin of bronchiectasis could not be concluded. In addition, bronchiectasis has a silent course and does not affect respiratory function tests.
To cite this abstract in AMA style:
Retuerto Guerrero M, Moriano C, Perez Garcia P, sieiro santos c, Diez álvarez e. Behind the Bronchiectasis in Systemic Sclerosis. Prevalence and Risk Factors [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/behind-the-bronchiectasis-in-systemic-sclerosis-prevalence-and-risk-factors/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/behind-the-bronchiectasis-in-systemic-sclerosis-prevalence-and-risk-factors/