Session Information
Session Type: Poster Session C
Session Time: 1:00PM-3:00PM
Background/Purpose: Sjogren’s Disease (SjD) is a heterogenous autoimmune disease associated with debilitating symptoms. Autonomic dysfunction (AD) is common in SjD and may contribute to symptom burden. We sought to compare AD symptom severity in SjD patients to those with FMS and healthy controls and implemented a patient-based stratification method to assess if AD is more prominent in certain subsets.
Methods: This is a cross-sectional study of SjD and FMS patients recruited in our Sjogren’s center between December 2021 and March 2022. Patients fulfilled 2016 ACR-EULAR criteria and FMS Survey Diagnostic Criteria and Severity Scale, respectively. Demographic, clinical, and laboratory variables were collected. A symptom-based stratification method was used to categorize SjD patients into 4 subgroups, based on the severity of pain, fatigue, dryness, anxiety, and depression, using Newcastle Sjogren’s Stratification software (available online at https://github.com/SJOGRENS/Symptom-Based-Subgroups), in which fatigue, dryness, and sicca symptoms were evaluated using EULAR’s Sjogren’s Syndrome Patient Reported Index (ESSPRI), while Hospital Anxiety and Depression Scoring (HADS) was used to assess anxiety and depression. Mean COMPASS-31 scores were compared between SjD, fibromyalgia groups, and historical controls (n=30) using previously published data. We also assessed COMPASS-31 scores in SjD subgroups and studied the association with clinical and laboratory variables, particularly in relation to the anti-SSA and SSB status.
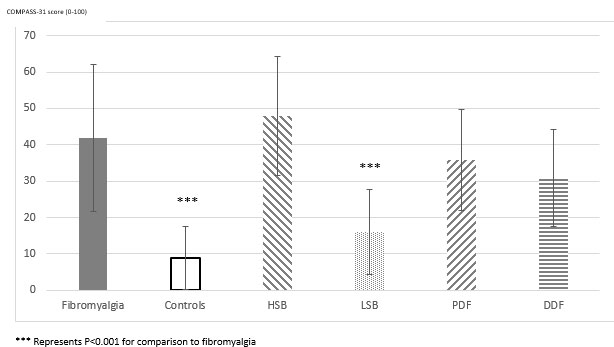
Results: 62 consecutive SjD and 20 FMS patients were recruited. The mean age for SjD patients was 55 years, with a mean disease duration of 8.3 years. Fifty-two (84%) were female. The mean COMPASS-31 score was significantly higher in SjD patients, compared to healthy controls (30.8±16.7 vs 8.9±8.7, p < 0.0001), but lower compared to FMS patients (30.8±16.7 vs 41.9±20.3, p=0.0169). Of 62 SjD patients, 8 were classified as high symptom burden (HSB), 16 as low symptom burden (LSB), 20 as pain dominant with fatigue (PDF), and 18 as dryness dominant with fatigue (DDF). COMPASS-31 score inversely correlated with Sjogren’s serotype and was the highest in the seronegative group (Table 1). COMPASS-31 score was highest in the high symptom burden subgroup (Figure 1).
Conclusion: To our knowledge, this is the first study that assesses AD in SjD using COMPASS-31 in comparison to FMS patients and a healthy population. Higher COMPASS-31 was observed in seronegative patients and those with the highest symptom burden, highlighting that AD may be implicated in symptom burden beyond the common symptoms of fatigue, dryness, and pain.
To cite this abstract in AMA style:
Fenando A, Estes J, Mohamad M, Shah S, Lee J, Jabari D, Baker J, Noaiseh G. Autonomic Dysfunction in Sjogren’s Disease [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/autonomic-dysfunction-in-sjogrens-disease/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/autonomic-dysfunction-in-sjogrens-disease/