Session Information
Date: Friday, November 6, 2020
Title: SLE – Diagnosis, Manifestations, & Outcomes Poster I: Clinical Manifestations
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Systemic Lupus Erythematosus (SLE) is a multisystem autoimmune disease. African ancestry is associated with an increased risk of Lupus Nephritis (LN). Anti-DNA autoantibodies play a major role in the development of LN and anti-Ro antibodies have also been implicated. McCarty et al suggested that women of African ancestry with the unusual autoantibody combination of anti-Sm, Ro & RNP antibodies (AB) were at increased risk of developing LN (1).
Our aim was to determine the correlation between autoantibody profile: Sm, Ro and RNP as a combination in the development of LN in patients with African ancestry. We investigated time to the development of LN from SLE onset.
Methods: A retrospective case-control study was conducted at Guys and St Thomas NHS Trust, London, United Kingdom.
84 patients with confirmed LN meeting the ACR classification criteria for SLE and Nephritis, were included: African (n=41), Caucasian (n=25) and Asian (n=18) ancestry. LN patients with the combination of Sm, Ro and RNP antibodies (Group 1) were compared to LN patients without this autoantibody combination (Group 2). Demographic data, pathology results and laboratory findings were collected.
P-values < 0.01 were considered statistically significant. All Anonymized data was analyzed using Statistical Package for Social Sciences (SPSS). Left censorship bias was reduced by use of a database of confirmed LN in our cohort of patients. Research and Development Office approval was obtained for this study.
Results: 84 patients were analyzed, females accounted for 75(89.3%) while males accounted for 9(10.7%), the median range was 44 y.o.
We stratified our population based on their antibody status: Of the 84 (100%) patients, 35 (41.7%) patients had the combination of Sm, Ro & RNP antibodies (Group 1) while the remaining 49 (58.3%) patients did not (Group 2).
In Group 1, regardless of ethnicity, 30 (85.7%) patients developed LN within 5 years or less from the onset of SLE symptoms, while the remaining 5 (14.3%) developed LN after 5 years. In contrast, in Group 2, 26 (53.06%) patients developed LN within 5 years or less while 23 (46.93%) developed LN after 5 years. (P value = 0.002)
Further stratification was based on ethnicity and antibody (AB) status to investigate the time to develop LN from SLE symptom onset: African ancestry with positive AB, African with negative AB, Asian with positive AB, Caucasian with positive AB and Asian & Caucasian with negative Ab. Analysis showed that out of 84 (100%) patients, 20(35.7%) African ethnicity patients with the positive autoantibody combination have developed LN in less than 5 years exceeding the number of those of other ethnic backgrounds. (P value = 0.01).
Conclusion: Patients with the unusual autoantibody combination of Sm, Ro & RNP developed LN significantly earlier than patients who did not have this combination. This autoantibody combination was significantly over represented in the African ancestry patients. Our data suggests that African ancestry patients with this autoantibody combination are at increased risk of developing LN soon after SLE symptom onset and merit close monitoring for the development of renal disease.
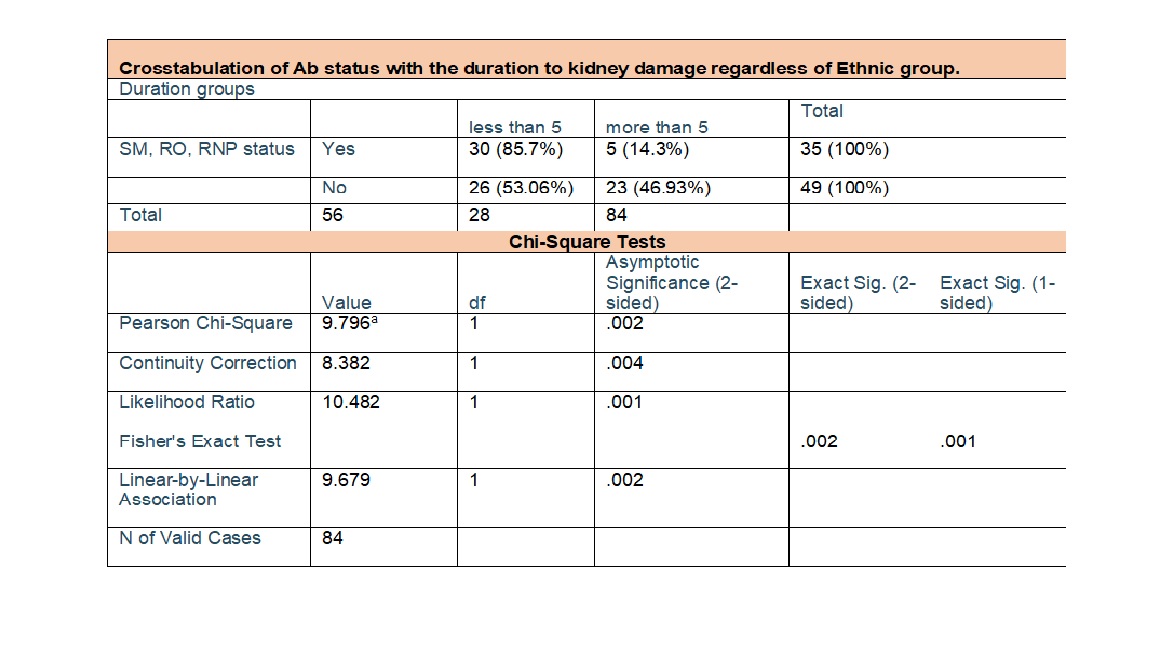 Table.1 Crosstabulation of Ab status with the duration to kidney damage regardless of Ethnic group P value= 0.002
Table.1 Crosstabulation of Ab status with the duration to kidney damage regardless of Ethnic group P value= 0.002
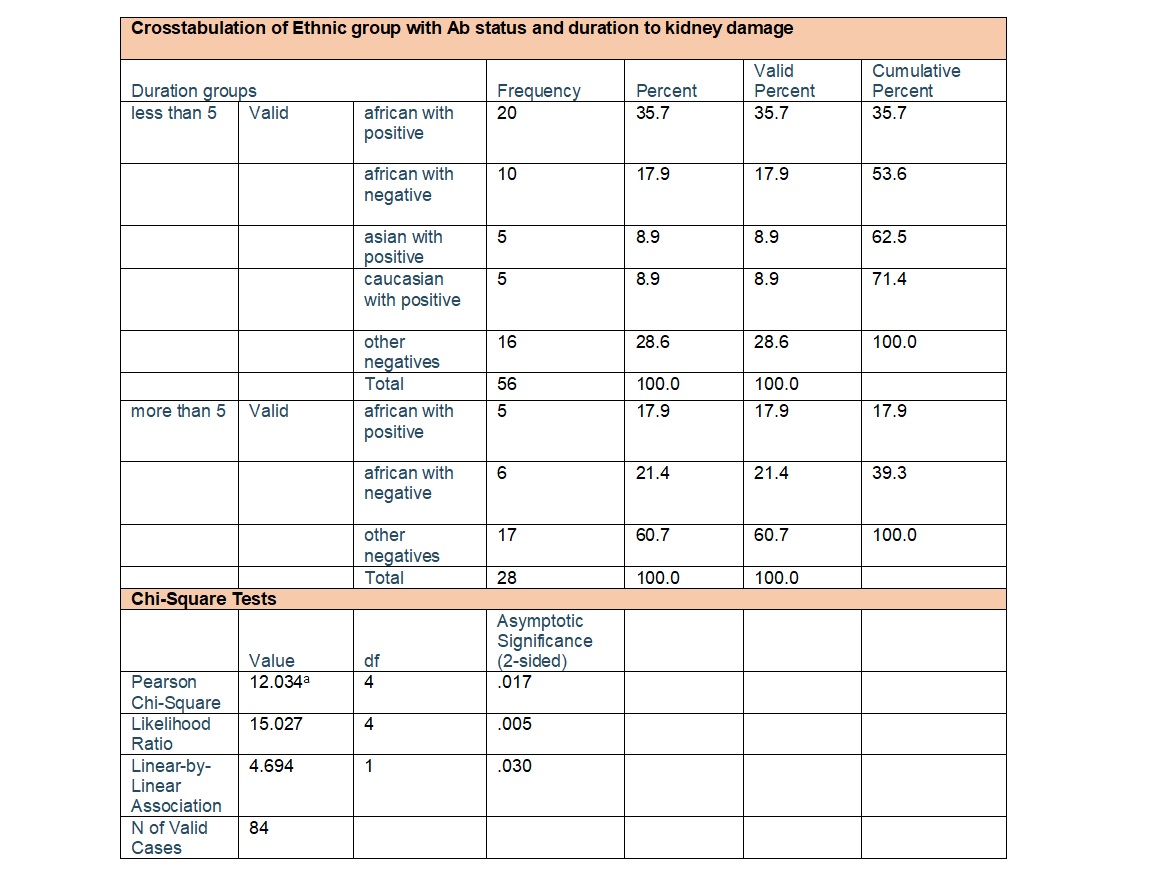 Table.2 Crosstabulation of Ethnic group with Ab status and duration to kidney damage P value= 0.017
Table.2 Crosstabulation of Ethnic group with Ab status and duration to kidney damage P value= 0.017
 Graph.1 Kaplan-Meier survival plot
Graph.1 Kaplan-Meier survival plot
To cite this abstract in AMA style:
Albirdisi M, d'Cruz D, Sangle S, Jordan N. Autoantibody Profile and Ethnicity: Risk Factors for Accelerated Development of Lupus Nephritis [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/autoantibody-profile-and-ethnicity-risk-factors-for-accelerated-development-of-lupus-nephritis/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/autoantibody-profile-and-ethnicity-risk-factors-for-accelerated-development-of-lupus-nephritis/
