Session Information
Session Type: Abstract Session
Session Time: 2:00PM-3:30PM
Background/Purpose: Upon activation with interferon (IFN) and RNP-immune complexes, defective mitophagy in neutrophils results in the release of mtDNA in complex with transcription factor A mitochondria (TFAM), leading to immune activation in SLE. TFAM is a member of the high-mobility group (HMG) family of DNA-binding proteins, which is essential for mtDNA transcription and for packaging mtDNA into nucleoids. Extracellular TFAM released from necrotic cells is also a DAMP. While characterizing novel autoantigens expressed by neutrophils, we identified TFAM as a target of antibodies in SLE. The purpose of this study was to investigate the relationship between anti-TFAM antibodies and clinical and transcriptional markers of disease activity in SLE
Methods: Anti-neutrophil antibodies in SLE sera were detected by indirect immunofluorescence (IIF). Anti-TFAM antibodies were screened by ELISA in sera from 98 healthy controls and 158 SLE patients from the “Study of biological Pathways, Disease Activity and Response markers in patients with Systemic Lupus Erythematosus” (SPARE). SPARE is a 2-year prospective cohort of adult patients for which extensive clinical, serologic, and whole blood transcriptional data is available. Binding of anti-TFAM antibodies to activated (GM-CSF + LPS) and necrotic neutrophils was determined by IIF.
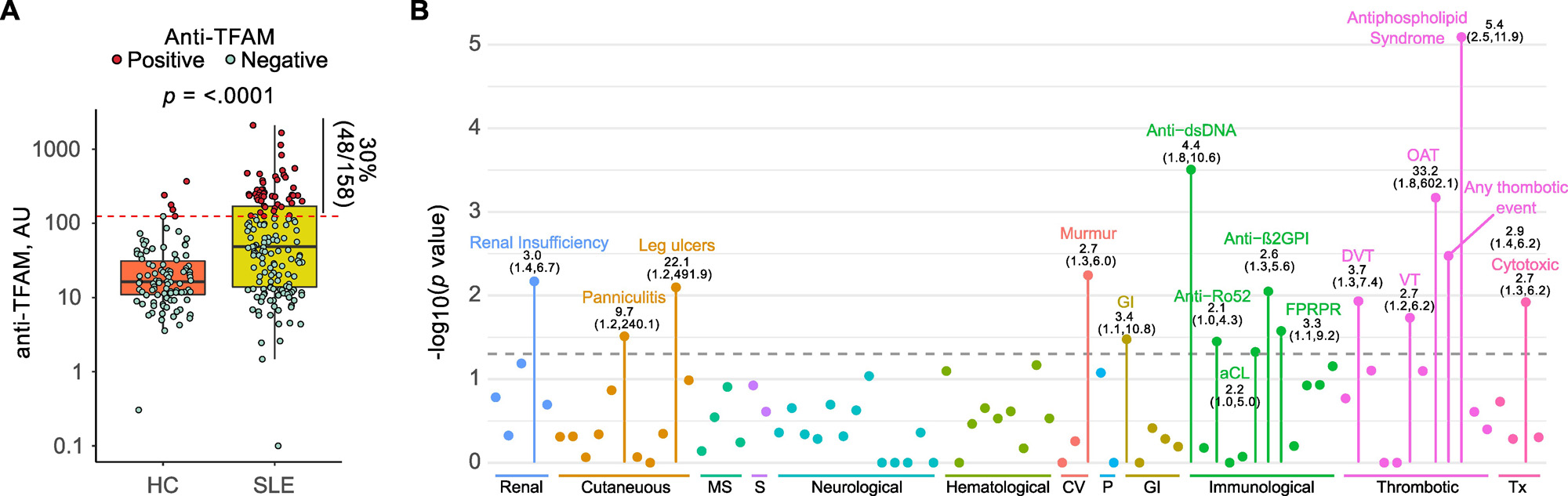
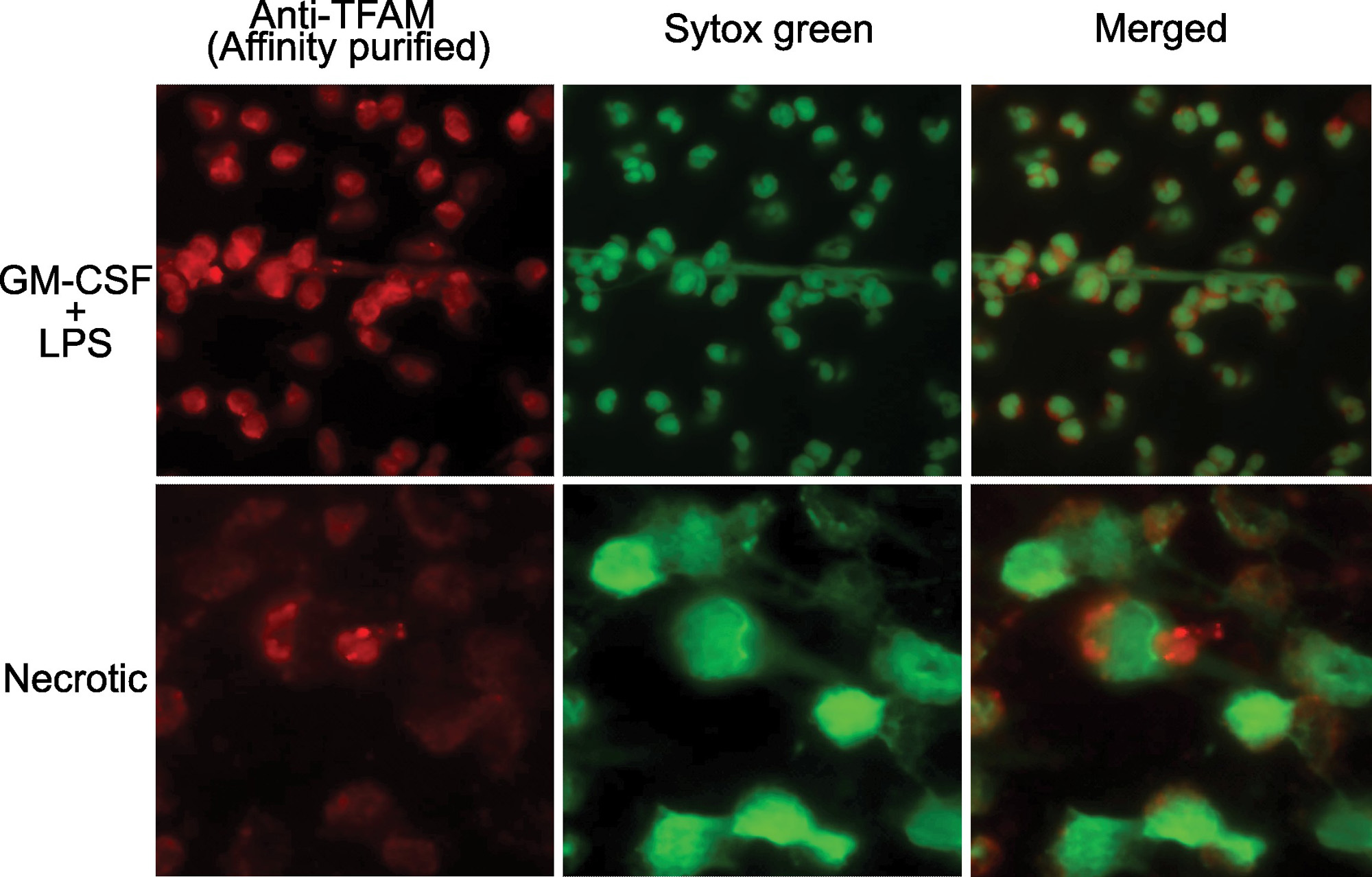
Results: A subset of antibodies in SLE serum co-localizes with TFAM in neutrophils. The existence of anti-TFAM antibodies in SLE was confirmed by ELISA and immunoblotting. Thirty percent (48/158) of SLE patients were positive for anti-TFAM antibodies (Fig. 1A). Anti-TFAM antibodies were significantly associated with antibodies to dsDNA, cardiolipin (aCL), and β2-glycoprotein I (β2GPI) (Fig 1B). Anti-TFAM antibodies were strongly associated with history of thrombotic events, OR (95% CI) 2.9 (1.4,6.2), and secondary antiphospholipid syndrome (APS), OR (95% CI) 5.4 (2.5,11.9), independently of aCL and anti- β2GPI (Fig. 1B). Unlike antibodies to dsDNA and RNPs, anti-TFAM antibodies were not associated with blood transcriptional markers of SLE disease activity, including the IFN signature, supporting a primary role of anti-TFAM antibodies in thrombosis rather than disease flaring. Anti-TFAM antibodies bind to TFAM-decorated DNA released from activated and necrotic neutrophils (Fig. 2), which is a mechanism that may contribute to thrombosis.
Conclusion: TFAM is novel autoantigen in SLE, which is associated with thrombosis and APS independently of aCL in SLE. These data support a link between mitochondrial damage and thrombosis in SLE.
To cite this abstract in AMA style:
Gomez-Banuelos E, Celia A, Trejo Zambrano M, Paz M, Darrah E, Goldman D, Petri M, Andrade F. Autoantibodies to Transcription Factor a Mitochondria Link Mitochondrial Damage and Thrombosis in Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/autoantibodies-to-transcription-factor-a-mitochondria-link-mitochondrial-damage-and-thrombosis-in-systemic-lupus-erythematosus/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/autoantibodies-to-transcription-factor-a-mitochondria-link-mitochondrial-damage-and-thrombosis-in-systemic-lupus-erythematosus/