Session Information
Date: Sunday, November 17, 2024
Title: Abstracts: SLE – Diagnosis, Manifestations, & Outcomes II: Biomarkers
Session Type: Abstract Session
Session Time: 1:00PM-2:30PM
Background/Purpose: We recently identified autoantibodies in SLE that target transcription factor A mitochondrial (TFAM), a critical protein in mitochondrial DNA transcription and packaging1. These autoantibodies are strongly associated to vascular events and antiphospholipid syndrome (APS) in SLE, independent of APS-associated antibodies or lupus anticoagulant. Given that vascular events play a significant role in the accumulation of damage and higher death rates in SLE, we investigated the potential role of anti-TFAM antibodies as predictors of damage accrual, and mortality in SLE.
Methods: We screened sera from 158 SLE patients in the “Study of biological Pathways, Disease Activity and Response markers in patients with Systemic Lupus Erythematosus” (SPARE) for anti-TFAM antibodies. SPARE is a 2-year prospective cohort of adult patients treated according to standard clinical practice. In addition, we measured normal anti-TFAM antibody levels in 98 healthy controls (HC). Damage accrual was measured using the Systemic Lupus International Collaborating clinics/American College of Rheumatology Damage (SLICC). Mortality and malignancy data were collected from the National Death Index and clinical charts, respectively.
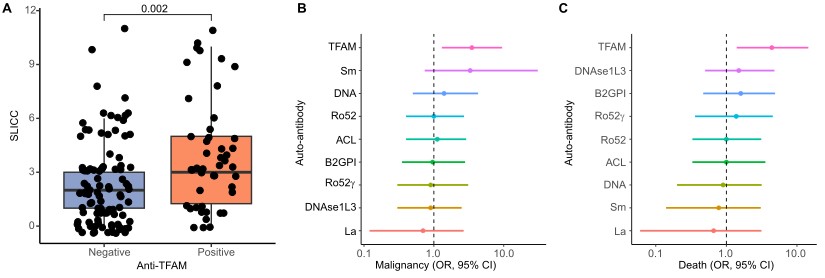
Results: Thirty percent (48/158) of SLE patients were positive for anti-TFAM antibodies. Anti-TFAM positive patients had higher SLICC scores compared to anti-TFAM negative patients (3.9 vs 2.3) (Fig 1A). Malignancy was the most frequent subdomain linked with elevated SLICC in anti-TFAM positive patients (29%), followed by diabetes mellitus (21%), ruptured tendon (15%), pericarditis (8%), muscular atrophy (8%), skin ulcers (8%), and deep vein thrombosis (6%). Among other SLE-related autoantibodies (Fig 1B), only anti-TFAM antibodies were associated with a greater risk of malignancy (OR 3.5). Anti-TFAM antibodies were not linked to any specific type of cancer. Intriguingly, there was no association between malignancy and thrombotic events in anti-TFAM positive patients. Furthermore, 23% (11/47) of anti-TFAM SLE patients died during follow-up (OR 4.4, Fig 1C). The most common cause of death in anti-TFAM positive SLE were cardiovascular related in 36% (4/11).
Conclusion: Anti-TFAM antibodies identify a subset of patients with SLE at higher risk for unfavorable outcomes, including malignancy and death. The lack of association between malignancy and thrombotic events in anti-TFAM positive patients suggests the existence of at least two subsets of anti-TFAM antibodies of distinct significance (i.e., thrombosis-related vs. cancer-related). The higher mortality among anti-TFAM positive SLE patients, with cardiovascular causes being the leading factor, highlights the importance of developing targeted interventions to prevent adverse outcomes in patients with anti-TFAM antibodies.
1.Gomez-Banuelos E, et.al. Autoantibodies to Transcription Factor a Mitochondria Link Mitochondrial Damage and Thrombosis in Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/autoantibodies-to-transcription-factor-a-mitochondria-link-mitochondrial-damage-and-thrombosis-in-systemic-lupus-erythematosus
To cite this abstract in AMA style:
Gomez E, Goldman D, Paz M, Petri M, Andrade F. Autoantibodies to Transcription Factor a Mitochondria Are Associated with Damage Accrual, Malignancy Risk and Mortality in SLE [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/autoantibodies-to-transcription-factor-a-mitochondria-are-associated-with-damage-accrual-malignancy-risk-and-mortality-in-sle/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/autoantibodies-to-transcription-factor-a-mitochondria-are-associated-with-damage-accrual-malignancy-risk-and-mortality-in-sle/