Session Information
Date: Friday, November 6, 2020
Title: RA – Diagnosis, Manifestations, & Outcomes Poster I: Multimorbidity
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Although a treat-to-target strategy is endorsed in rheumatoid arthritis (RA) treatment guidelines, its routine implementation in real-world settings, particularly in the context of multimorbidity, is not well understood. In this study, we examined whether multimorbidity is associated with DMARD initiation and the achievement of target disease activity thresholds in patients with RA using the largest Electronic Health Record-enabled rheumatology registry in the U.S.
Methods: We conducted a retrospective cohort study within the Rheumatology Informatics System for Effectiveness (RISE) registry. We selected patients >18 years of age, with ≥2 encounters for RA based on ICD-10 codes, and who had 2 consecutive visits in moderate or high disease activity (by Clinical Disease Activity Index [CDAI] or Routine Assessment of Patient Index Data 3 [RAPID3]) without treatment changes between visits. For inclusion in analyses assessing treatment response, we additionally required initiation of a new DMARD at or immediately following the 2nd visit and ≥1 additional visit in the following 365 days. Demographics, seropositivity, disease activity, and medications were obtained from the RISE registry. Multimorbidity was measured using RxRisk, a medication-based index of chronic disease, and modeled both as a continuous variable and categorized into quartiles based on the number of RxRisk categories using all available prior medication data. We used multivariable logistic regression models to assess the independent associations of multimorbidity with 1) the odds of initiating a new DMARD in active RA; and 2) among those initiating a new DMARD, the odds of achieving low disease activity or remission. Separate models were constructed for CDAI and RAPID3 cohorts.
Results: We identified 15,626 (RAPID3) and 5,733 (CDAI) patients with active RA, of which 1,558 (RAPID3) and 834 (CDAI) initiated a new DMARD and had ≥1 follow-up visit within 365 days. Patients were middle aged, female and Caucasian predominant, and frequently received medications from ≥5 RxRisk categories (Table 1). Multimorbidity was not independently associated with the odds of initiating a new DMARD in the setting of active RA in either the RAPID3 or CDAI cohorts (Table 2). However, among RA patients with active disease initiating a new DMARD, greater multimorbidity burden was associated with a lower likelihood of achieving low disease activity or remission (Table 3). Patients with the highest burden of multimorbidity (≥12 RxRisk categories) had approximately half the odds of achieving target RA disease activity (OR=0.48 RAPID3; OR=0.55 CDAI) compared to those with ≤5 RxRisk categories.
Conclusion: After initiating a new therapy for active RA, patients with greater multimorbidity were less likely to achieve target RA disease activity. These findings from a large, real-world registry illustrate the potential impact of multimorbidity on treatment response and indicate that broader management efforts targeted at multimorbidity may be needed to optimize RA disease control in these patients. Comparative effectiveness studies in multimorbid RA patients are needed since the risks and benefits of therapies may differ in this population.
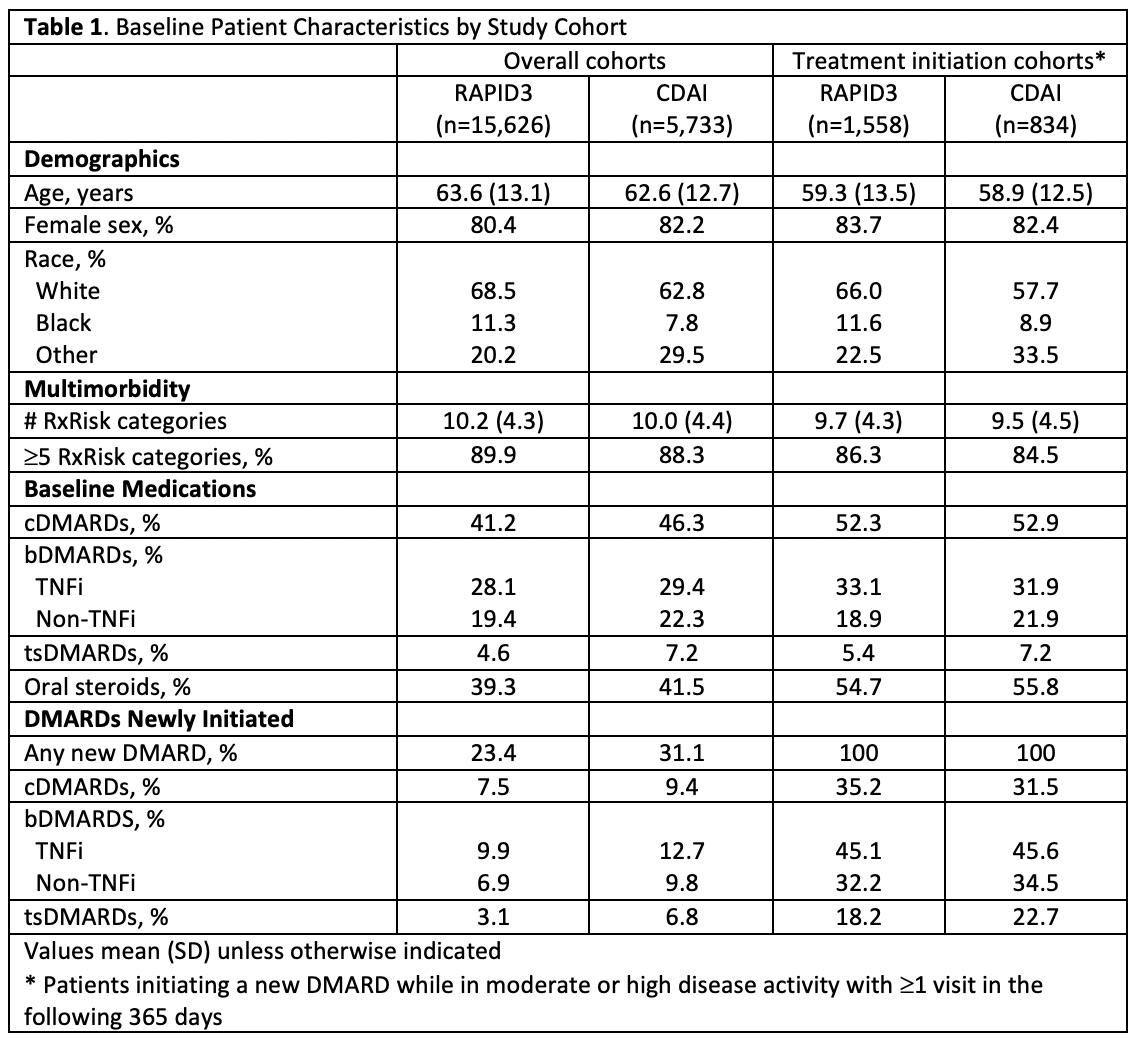 Table 1. Baseline Patient Characteristics by Study Cohort
Table 1. Baseline Patient Characteristics by Study Cohort
 Table 2. Association of Multimorbidity with Initiating a New Treatment in Active RA
Table 2. Association of Multimorbidity with Initiating a New Treatment in Active RA
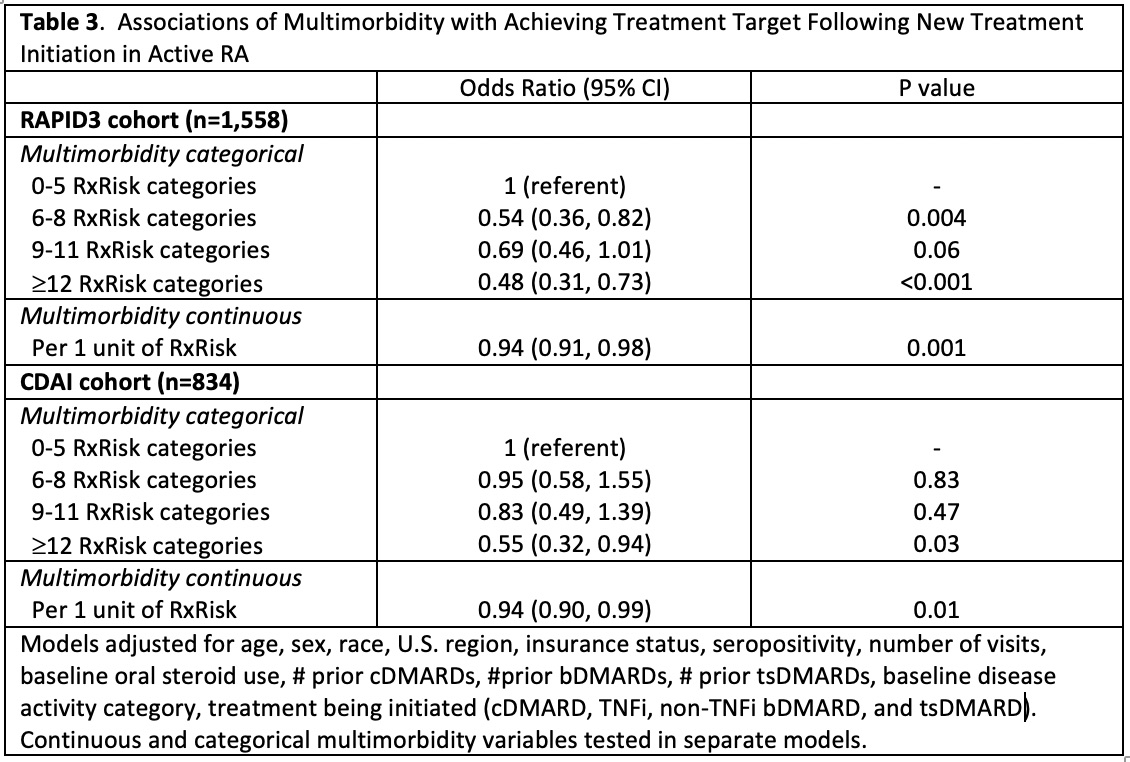 Table 3. Associations of Multimorbidity with Achieving Treatment Target Following New Treatment Initiation in Active RA
Table 3. Associations of Multimorbidity with Achieving Treatment Target Following New Treatment Initiation in Active RA
To cite this abstract in AMA style:
England B, Yun H, Chen L, Michaud K, Mikuls T, Curtis J. Associations of Multimorbidity with DMARD Initiation and Achieving Target Disease Activity Thresholds in Active Rheumatoid Arthritis: A Cohort Study Using the Rheumatology Informatics System for Effectiveness (RISE) Registry [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/associations-of-multimorbidity-with-dmard-initiation-and-achieving-target-disease-activity-thresholds-in-active-rheumatoid-arthritis-a-cohort-study-using-the-rheumatology-informatics-system-for-effec/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/associations-of-multimorbidity-with-dmard-initiation-and-achieving-target-disease-activity-thresholds-in-active-rheumatoid-arthritis-a-cohort-study-using-the-rheumatology-informatics-system-for-effec/
