Session Information
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Wildfires have burned increasing acreage in the United States (US) since the 1980s, releasing record and alarming levels of particulate matter smaller than 2.5 microns (PM2.5,). In addition, respiratory tract irritation is associated with rheumatoid arthritis (RA). Therefore, we aimed (1) to determine the associations between fire smoke PM2.5 and other pollutant exposures with the risk of RA and RA-associated interstitial lung disease (RA-ILD) and (2) to identify the timing of any such associations.
Methods: In this case-control study using national Veterans Affairs (VA) data, we identified incident RA and RA-ILD cases using validated algorithms (positive predictive values >90% and 81%, respectively). We matched each case to up to 10 controls on age, gender, and VA enrollment year. Seropositivity was based on electronic health record laboratory data. The primary exposure was mean daily fire smoke PM2.5 at least one year before RA diagnosis, obtained from a fused product of ground pollutant monitoring and satellite imagery. Other pollutants included carbon monoxide, nitrogen oxides (NOx), ozone, overall PM2.5, PM10, and sulfur dioxide (SO2). Pollutant exposures were also evaluated by time periods before RA (1-3 years, 3-5 years, >5 years). We used conditional logistic regression models to estimate adjusted odds ratios (aOR) with 95% confidence intervals (CI) for incident RA and RA-ILD, adjusted for age, gender, enrollment year, duration of pollutant exposures, race and ethnicity, body mass index, and smoking status.
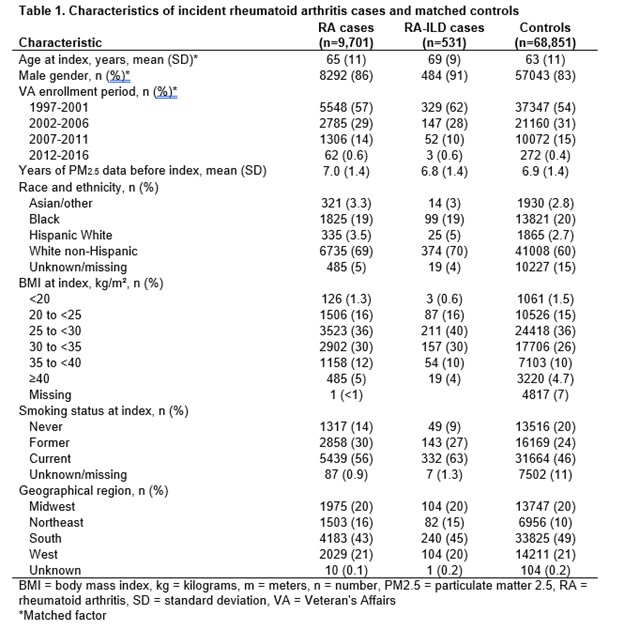
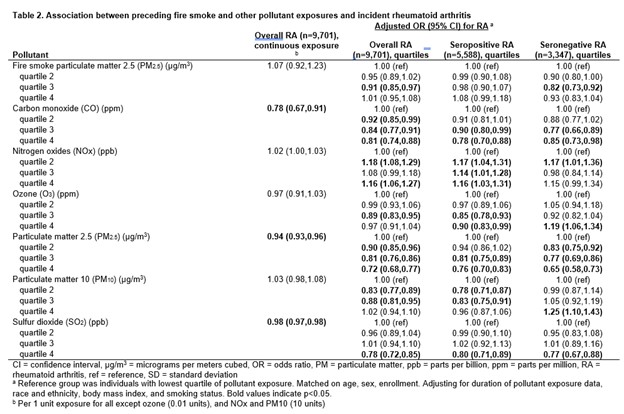
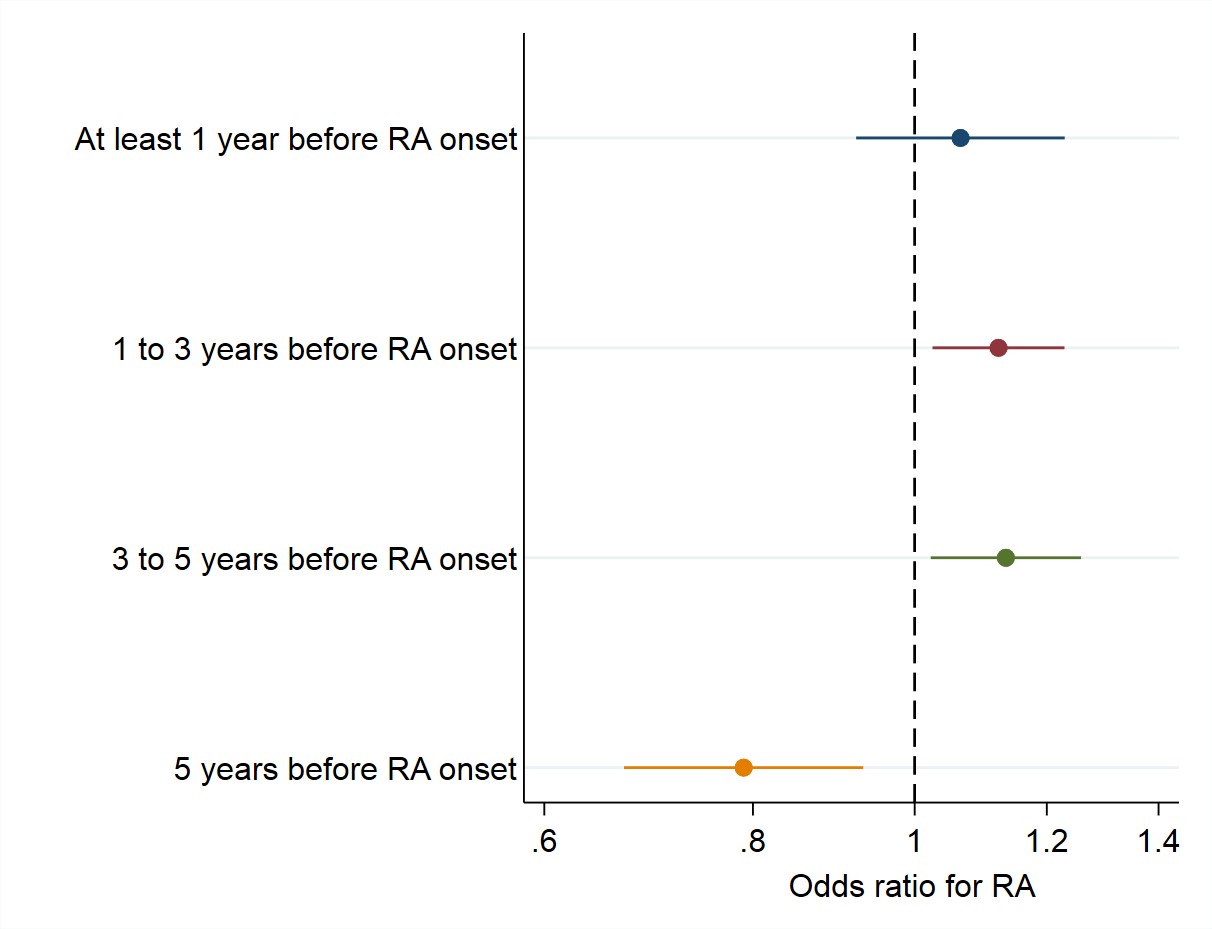
Results: We identified 9,701 incident RA cases (mean age 65, 86% male), including 531 RA-ILD cases (mean age 69, 91% male), and 68,852 matched controls (Table 1). Fire smoke PM2.5 was not associated with RA overall (aOR 1.07, 95% CI 0.92-1.23, Table 2), but was associated in the 1-5 years before RA onset (aOR 1.13, 95% CI 1.02-1.26, Figure 1). Fire smoke PM2.5 was associated with RA-ILD (aOR 1.98, 95% CI 1.08-3.62 per 1 µg/m3). Increased levels of NOx were also associated with RA (aOR 1.16, 95% CI 1.06-1.27 for highest vs. lowest quartile, Table 2). Ozone (aOR 1.19, 95% CI 1.06-1.34) and PM10 (aOR 1.25, 95% CI 1.10-1.43) were associated with seronegative, but not seropositive, RA. Carbon monoxide, overall PM2.5, and SO2 were not, or negatively, associated with risk of RA and RA-ILD (Table 2).
Conclusion: Increased levels of fire smoke PM2.5 are associated with RA-ILD, while fossil fuel-related NOx, ozone, and PM10 are associated with RA. Therefore, improved pollutant monitoring infrastructure and prevention strategies are needed.
Disclosures: V. Kronzer: None; Y. Yang: None; P. Roul: None; J. Crooks: None; C. Crowson: None; J. Davis: Girihlet, 10, NLC Health Ventures, 10, Pfizer, 5, Remission Medical, 10; J. Sparks: Boehringer-Ingelheim, 2, 5, Bristol-Myers Squibb(BMS), 2, 5, Gilead, 2, Janssen, 2, Pfizer, 2, UCB, 2; J. Pierce: None; K. O'Dell: None; S. brian: None; g. Cannon: None; J. Baker: CorEvitas, LLC, 2, Cumberland Pharma, 2, Formation Bio, 2, Horizon, 5; T. Mikuls: Elsevier, 9, Horizon Therapeutics, 2, 5, Pfizer, 2, Sanofi, 2, UCB Pharma, 2, Wolters Kluwer Health (UpToDate), 9; B. England: Boehringer-Ingelheim, 5.
To cite this abstract in AMA style:
Kronzer V, Yang Y, Roul P, Crooks J, Crowson C, Davis J, Sparks J, Pierce J, O'Dell K, brian S, Cannon g, Baker J, Mikuls T, England B. Associations of Fire Smoke and Other Pollutants with Incident Rheumatoid Arthritis and Rheumatoid Arthritis-Associated Interstitial Lung Disease [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/associations-of-fire-smoke-and-other-pollutants-with-incident-rheumatoid-arthritis-and-rheumatoid-arthritis-associated-interstitial-lung-disease/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/associations-of-fire-smoke-and-other-pollutants-with-incident-rheumatoid-arthritis-and-rheumatoid-arthritis-associated-interstitial-lung-disease/