Session Information
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Alterations in the gastrointestinal (GI) microbiome (i.e., dysbiosis) are a feature of systemic sclerosis (SSc) [1]. Diet is a known modifier of the GI microbiome, and ultra-processed food (UPF) consumption, specifically, has been associated with adverse changes in GI microbial composition [2]. This study aimed to determine whether UPF consumption affects the GI microbiota and symptoms in patients with SSc.
Methods: Adult SSc patients provided stool samples and completed both the Diet History Questionnaire II (DHQ-2) and the UCLA Scleroderma Clinical Trial Consortium Gastrointestinal Tract Instrument (GIT 2.0). Shotgun metagenomics were performed using the Illumina NovaSeq 6000 with a target depth of 20 million 150×2 sequences per sample. Shotgun reads were inputted into MetaPh1An2 for taxonomic identification of species for compositional analysis, and samples were filtered to retain species with at least 25% non-zero counts. UPF items (N=54) on the DHQ-2 were identified using the NOVA scale of food classification [3]. UPF intake was calculated as a continuous variable by gram-per-week consumption according to patient reported frequency. General linear models were created to identify differentially abundant species based on UPF consumption and to evaluate the relationship between UPF consumption and GI symptoms as measured by the GIT 2.0. These models adjusted for body mass index (BMI), current proton pump inhibitor (PPI) use, current probiotic use, current or prior immunomodulatory therapy, and presence of small intestinal bacterial overgrowth (SIBO). The False Discovery Rate (FDR) was used to correct for multiple hypothesis testing.
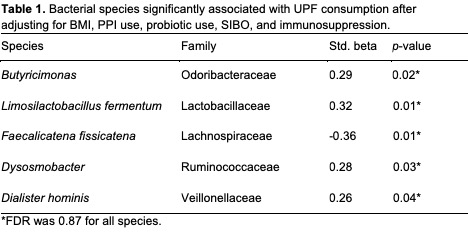
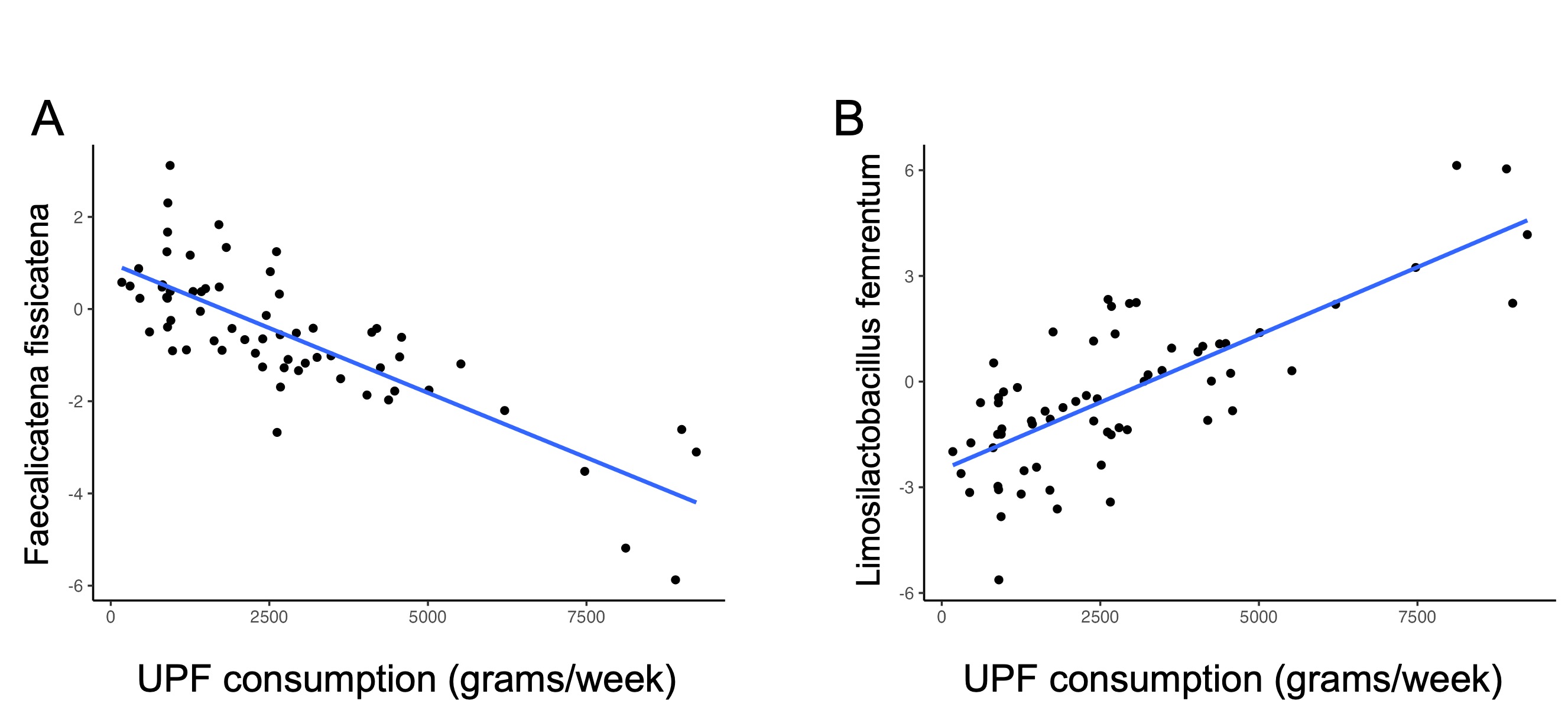
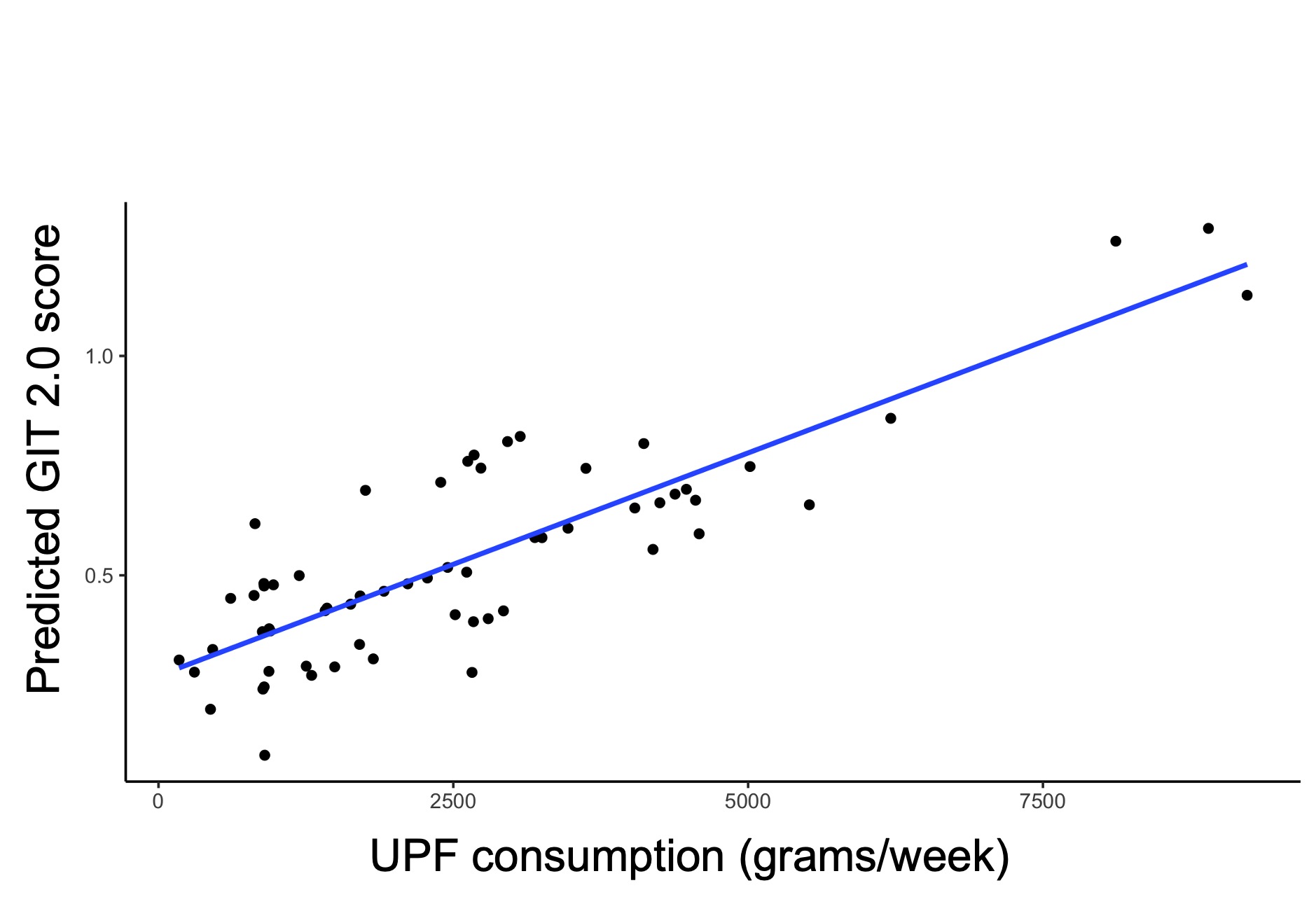
Results: Of the 65 total SSc patients included, 59 were female (90.7%). The mean age was 53.25 years (SD=12.84), and the mean BMI was 25.7 (SD=4.88). The median UPF consumption was 2394.5 grams/week with a range of 174.5-46978.2 grams/week. Among 257 species analyzed, the abundance of 10 bacterial species was significantly altered based on UPF consumption in study participants. After adjusting for the aforementioned covariates, 5 bacterial species were significantly associated with UPF consumption [Table 1], including Limosilactobacillus fermentum (Std-beta 0.32; p< 0.01) [Figure 1A] and Faecalicatena fissicatena (Std-beta -0.35; p< 0.01) [Figure 1B]. Increased UPF intake was significantly associated with GI symptoms in the multivariable model (Std-beta 0.34; p< 0.01) [Figure 2].
Conclusion: SSc patients reporting a higher UPF consumption demonstrated alterations in GI microbial composition as well as increased GI symptoms, even after adjusting for factors known to affect the microbiota of patients with SSc. Future studies are needed to determine whether interventions aimed at lowering UPF consumption may improve GI outcomes for patients with SSc.
1. Andréasson K, et al. ACR Open Rheumatol 2022;4(5):417-425.
2. Chassaing B, et al. Gut 2017;66(8):1414-1427
3. Monteiro CA, et al. Public Health Nutr 2018;21(1):5-17.
To cite this abstract in AMA style:
Lee J, Joshi S, Young A, Labus J, McMahan Z, Aja E, Jacobs J, Volkmann E. Associations Between the Gut Microbiota, Ultra-Processed Food Intake, and Gastrointestinal Tract Symptoms in Patients with Systemic Sclerosis [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/associations-between-the-gut-microbiota-ultra-processed-food-intake-and-gastrointestinal-tract-symptoms-in-patients-with-systemic-sclerosis/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/associations-between-the-gut-microbiota-ultra-processed-food-intake-and-gastrointestinal-tract-symptoms-in-patients-with-systemic-sclerosis/